The study, reported in Vaccine, reviews a survey of Arizonians, part of the Arizona COVID-19 Cohort (CoVHORT). Given that:
- Vaccines and boosters for COVID have reduced hospitalization, disease severity, death, and the risk of Long COVID
- These vaccines and natural immunity wanes over time
Why would less than 20% of those eligible receive an updated booster?
The common narrative for the reasons is a tangle of misinformation, political affiliation, and anti-vaxx sentiments. In a separate study, roughly a quarter of the U.S. population supported vaccines “with concerns,” 25% were vaccine-hesitant, and 7% were anti-vaxx. From a public health perspective, we can ignore the anti-vaxx individuals; logical arguments will fail in the face of emotionally charged beliefs. However, 50% of concerned and hesitant may be moved towards a booster if their concerns can be addressed. As with all retail sales, the first step in that persuasion is to understand the consumers' objections.
The researchers sent surveys to all the CoVHORT participants; 48% responded, and those previously not vaccinated were excluded, leaving roughly 2,200 participants. 75% of those participants had been boosted, so the survey results reflect 560 participants not receiving the bivalent vaccine booster. [1]
Here is what they found:
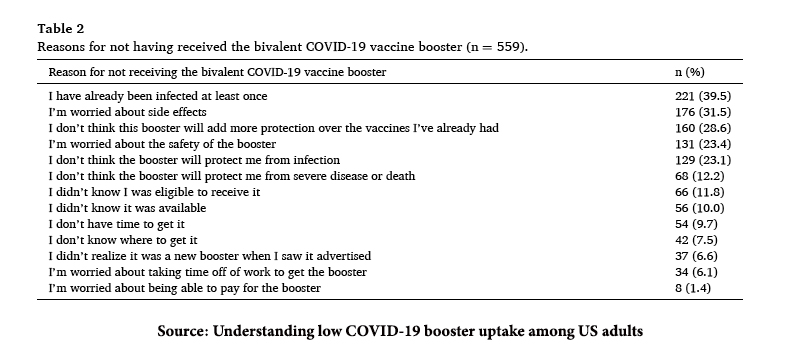
There are three themes here.
First, that having been infected or initially vaccinated is adequate protection. Public health messaging was late recognizing and reporting that infection-acquired immunity was real and robust. The emphatic messaging about getting initially vaccinated was predicated on the need to “flatten the curve” of hospitalization; infection-acquired immunity does little to flatten that curve. While detractors suggested that the “goalposts” of immunization moved during the pandemic, the greater truth is that the goalposts were ill-defined to the public. The second misunderstanding here concerns a less nuanced understanding of immunization. When considering vaccination, many of us think of polio or measles – a very different organism from COVID. Polio and measles vaccinations are one-and-done; relatively no need for a booster. But COVID is a respiratory virus, like influenza, an organism whose vaccination needs to be updated over time. Public health officials did little to explain the natural history of vaccines, so the waning efficacy, especially when compared to the emphatic certainty of the vaccine’s early success, was lost in translation – contributing to uncertainty and mistrust.
Second, there were concerns about side effects and safety. Because we were giving a new form of vaccination to a large population as quickly as possible, public health officials acted out of an abundance of caution. Remember, you had to stay at the vaccination center for 15 minutes of observation lest you develop an anaphylactic reaction to the vaccine. That 15-minute wait speaks to the power of the vaccine harm. As with all translations of clinical trials to public health measures, efficacy, and harm become more evident in the real world. That was certainly the case for side effects. Here, we might first look to the media, which at times, lumped a painful injection site and fatigue, in with more consequential side-effects. A bigger number gathers more attention, but fighting over those numbers made for “crying wolf,” making it more difficult for some to accept that weak but persistent signal of myocarditis in young men. Once again, we were misinformed primarily because while we began to know the numbers of those young men developing myocarditis, some would speak of this problem with a denominator of how often it was raised in the media versus how often it was seen in those vaccinated or infected. Denominator matters. In the context of repetition of mentions, the early reports create a more fearful number – which parenthetically feeds back to make more mentions. But when the denominator of those developing myocarditis from vaccination was compared to those with myocarditis from infection, this complication was not so fearsome. Of course, fear is difficult to squelch.
Third, there were issues of access. I am inclined to discount that concern because I remember the time spent and the ink spilled on describing the rush to initial vaccination – the lines, confusion, and hours spent on a computer trying to get an appointment. Getting that bivalent booster took nowhere near the time and effort.
The communication over COVID vaccination has been far less than ideal. It is due to a host of reasons, including governmental hubris, a citizenry with a low literacy for numbers and science, a social media more inclined to sensationalize than clarify, and fear. Convincing those with concerns, or those hesitant, can only be accomplished if we meet on their terms and discuss their fears as equals, not as parental experts. The next public health crisis will differ from the COVID pandemic, but how we talk to one another to reduce misinformation and mistrust will not.
[1] Just to be clear, the current vaccine offering is not a booster; it is a new vaccine directed at the present COVID variants of concern.
Source: Understanding low COVID-19 booster uptake among US adults Vaccine DOI: 10.1016/j.vaccine.2023.08.08




