A Church Choir Rehearsal
A COVID-19 outbreak occurred in March 2020 that provided a unique set of experimental data. Sixty-one choir members rehearsed in a relatively confined space, where singing would have increased their exhaled virus emission rates. Face masking would not have been practical in this situation, and vaccines were not available. They rehearsed for about 2.5 hours; 53 of them became infected with COVID-19 within five weeks, and 2 of them died. A modeling study of this event estimated viral emission rates, episode duration effects, and virus deposition rates to surfaces in the room. I extrapolated these results and estimated that a 5-hour exposure could have infected the entire group.
USS Theodore Roosevelt, March-May 2020
The Roosevelt is a nuclear-powered aircraft carrier with a crew of 4779 that began experiencing COVID-19 symptoms while in the Pacific. It docked at Guam, where everyone was tested, and those who tested positive (27%) were quarantined in single-occupancy hotel rooms. The 2-month total infection rate was similar to the current US pandemic-wide rate (30%). 77% of those who tested positive had no concurrent symptoms. For comparison, national infection rates were much lower at that time, typically around 100-1000 daily cases per million population.
Diamond Princess cruise ship, February 2020
A literature review of cruise ship outbreaks identified 79 voyages. I identified one significant event that was amenable to analysis. The COVID index case was on board from January 21-25, and 619 (17%) positive tests were reported among passengers and crew by February 20. This is consistent with the infectivity seen aboard the USS Roosevelt. Mathematical modeling estimated that earlier isolation and quarantining could have prevented about 60% of the cases.
Charles de Gaulle aircraft carrier, March-April 2020
This ship was on a 4-month cruise with several port visits. After an outbreak was observed, the crew was treated as a cohort. Officer status, physical distancing, and smoking reduced infection risks by about 40%. Flight-deck duty quadrupled the infection risk, attributed to proximity to the outbreak's origin. Hand-washing or sleeping arrangements had no statistical impact.
The Reykjavik outbreak, July 2, 2021
During a visit, this event involved an unnamed US Navy ship; 98% of the 350-person crew had been vaccinated. Masking, extra cleaning, and social distancing procedures had been relaxed. By August 7, 22 personnel (6.3%) had been infected with COVID; all of them were symptomatic, and there were no hospitalizations or deaths. The attack rate onboard ship was 2200 per million population, while the infection rate for vaccinated US civilians was 150 per million population at that time.
An airborne outbreak, March 2020
In flight transmission was reported for 16 passengers on a 10-hr Viet Nam Airlines flight. Infection risk was strongly associated with seating proximity.
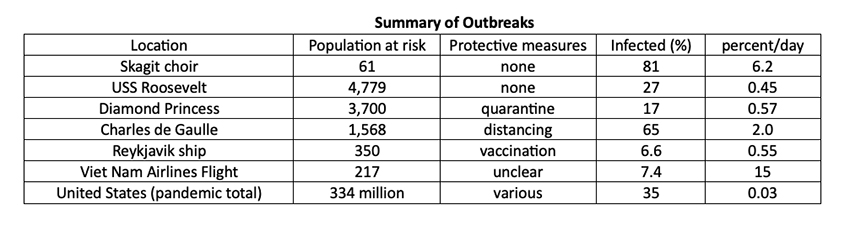
- The four shipboard outbreaks had similar daily infection rates despite differences in types of protective measures, illustrating the importance of prompt implementation of such protection.
- The ~12-fold difference between the church choir and shipboard outbreaks indicates the combined impacts of longer exposure durations and shorter separation distances for the choir members.
- The 20-fold ratio between shipboard infection rates and the US national average reflects potentially more significant social distancing, attenuation by face masks, and increased immunity from vaccination.
All of this information supports the conclusion that exhaled aerosol is the primary mode of virus transmission.
Hypothetical Exposure Indices
I hypothesized parameters for exposure modes concerning virus emission and reception to examine exposure relationships. I assumed that viral emission is proportional to respiration rate and duration of activity and inversely proportional to the separation distance. Room air exchange was not considered in this simple characterization. Notwithstanding uncertainties in these parameters, the duration of exposure and separation distances appear to be the most important.
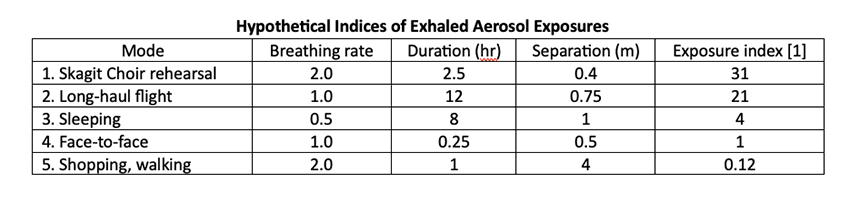
Face-to-face activities could be prolonged and are relatively more important. The potential 3 to 4-fold risk reductions from vaccination or face-masking pale in the context of the range of this 20 to 30-fold exposure variability. COVID outcomes have been highly variable during the pandemic, ostensibly because of new variants and difficulties implementing protective measures.
My analysis of these specific situations indicates that exposure is the critical factor amenable to individual control.
[1] I defined an exposure Index as b*t/d2 where b is respiratory rate, t is exposure duration, and d is separation distance. D is squared because exhalation will likely spread downwind as a cone rather than linearly as a jet.



