If elements could be diagnosed using the DSM-V, zinc would be a textbook case:Code F31.9 — Bipolar I Disorder, current or recent episode unspecified.
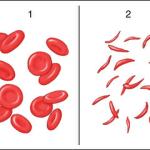
antibiotic resistance
"With the wrong metaphor we are deluded; with no metaphor we are blind."
- Jonathan Haidt, The Happiness Hypothesis
Scientists in Germany tested 94 substances on E. coli in a lab. They found that caffeine flips a switch in the bacteria called Rob, which makes it harder for certain antibiotics.
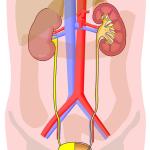
A breakthrough, almost decade-long study of a spray vaccine offers promise for hundreds of millions of women who suffer from urinary tract infections (UTIs) over their lifetimes.
In a lively exchange with Lars Larson, we dove headfirst into the realm of groundbreaking medical advancements, touching on the pressing issue of antibiotic resistance.
During my lifetime, there have been several seminal breakthroughs in medicine that greatly changed our ability to prevent or treat disease. Part 1, below, describes several of them. I have a good idea of what some of the next ones will be.
JB: A new report in USA Today is certainly looking for readers. The title clearly reflects this:
“Not 'if' but 'when': Antibiotic resistance poses an existential threat for modern medicine”
1211 participants underwent “clean” (a CDC definition of infectious nature of the surgery) orthopedic surgery, were given appropriate antibiotics within an hour of beginning surgery, and repeated every 3 to 4 hours during surgery.
Here we go again. Entasis Therapeutics has been struggling in the public marketplace.