Though the sciences of microbiology and public health have largely made infectious disease an afterthought for most people in the developed world, microbes have not gone away.
antibiotic resistance
Promising work just published in Nature Medicine especially offers hope to chronically ill patients battling drug-resistant infections while most compromised with weakened im
The headlines are rampant lately about “a mysterious and deadly fungal infection..spreading across the globe” that identifies multidrug-resistant yeast, Candida auris, as a “new fungal superbug.” And, as is common with such alarming heade
How often do you hear of someone using their spouse’s antibiotic medication that was prescribed for a prior illness but not entirely if ever used? Or, a teen sharing her friend’s birth control pills?
Ah, our body’s microbiome, the bacteria living in symbiotic harmony in our gut, that newly discovered source of wellness, its mysteries only slowly being revealed. Our microbiome is an inner ecology of Planet Us.
Urgent care centers and retail clinics top the list when it comes to the inappropriate use of antibiotics, according to a new study in JAMA Internal Medicine
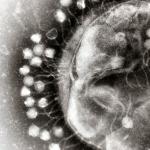
Even with the advent of the antibiotic era, infectious diseases are a global health concern.
I have been writing for years (1) about the emergence and spread of bacteria that are resistant to virtually all antibiotics, and that it was only a matter of time until they reached the US. Time's up.
Recently, I had the pleasure of filming a segment on the top medical, science and technology innovations of 2017 at Reuters TV in Times Square, New York with host of CCTV Bianca Chen.