Antibiotic-resistant bacteria cause more than two million infections per year in the US, resulting in ~23,000 deaths. These infections incur an estimated $20 billion in direct healthcare costs and $35 billion in lost productivity, and these costs are expected to rise rapidly over the next several years. The threat of antibiotic resistance is especially critical in the case of Gram-negative bacterial pathogens, such as Pseudomonas aeruginosa, Acinetobacter baumannii, and Klebsiella pneumoniae. Infections caused by MultiDrug Resistant (MDR) Gram-negative bacteria result in higher mortality rates, longer hospital stays and higher treatment costs compared to antibiotic-susceptible infections.
Patients with MDR Gram-negative bacterial infections have a mortality rate of 30-70%, which is approximately two to threefold higher than patients who have an antibiotic-susceptible infection. In 2005, there were 368,600 hospital stays with Methicillin Resistant Staphylococcus Aureus (MRSA) infections in the US, at a resulting cost of $5 billion. The incidence tripled between 2000 and 2005. Invasive MRSA resulted in 18,650 deaths in the US in 2005. The first case of MRSA appeared in 1961, just one year after the introduction of methicillin. MRSA was widespread in Europe by the end of the 70s and in the US by the end of the 80s. Nasal MRSA carriage is a major risk factor in hospital community infections. In 2002, 2 million hospital patients succumbed to hospital-acquired infection leading to 99,000 deaths.
The SUPERBUGS - WHO lists the following bacterial organisms that pose significant (re)-emerging threats to humans:
Three bacteria are considered to be of critical priority:
- Pseudomonas aeruginosa, carbapenem-resistant
- Enterobacteriaceae, carbapenem-resistant, ESBL-producing
- Acinetobacter baumannii, carbapenem-resistant
Six are considered to be of high priority:
- Enterococcus faecium, vancomycin-resistant
- Staphylococcus aureus, methicillin-resistant, vancomycin-intermediate and resistant
- Helicobacter pylori, clarithromycin-resistant
- several species of Campylobacter, fluoroquinolone-resistant
- Salmonellae, fluoroquinolone-resistant
- Neisseria gonorrhoeae, cephalosporin-resistant, fluoroquinolone-resistant
Three are deemed to be of medium priority:
- Streptococcus pneumoniae, penicillin-non-susceptible
- Haemophilus influenzae, ampicillin-resistant
- Several species of Shigella, fluoroquinolone-resistant
The biggest threat is the explosion of drug-resistant TB. More than 50 years after the introduction of the first of many successful anti-TB drugs, this disease remains a leading cause of death around the world. In 2013, 9 million people were infected with TB and 1.5 million died of the disease. That is an ongoing plague in anyone’s book. There were an estimated 450,000 new cases of multidrug resistant and extremely drug resistant TB infections in 2012 alone. We are witnessing outbreaks of drug resistant TB exhibiting mortality rates last seen in the pre-antibiotic era.
How did we get here? This problem has many fathers starting with this famous quote:
“It is time to close the book on infectious diseases, declare the war against pestilence won and…”
LBJ’s US Surgeon-General W. Stewart in 1967
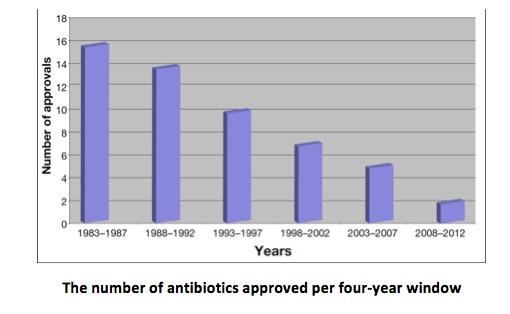
However, antibiotic resistance was as predictable as the sun rising. Resistance to penicillin in S. aureus was first seen in 1943 and within a few years after introduction of penicillin, more than 80% of the hospital isolates were resistant. The war against pestilence is a perpetually ongoing battle with no end, ever. Unfortunately, the pharmaceutical industry took Stewart’s quote to heart and began to abandon this part of the drug invention business starting in the 80s. In 1990 there were 20 companies doing antibiotic R&D; today only 2 remain. New clinical trial requirements were established by the FDA in the 1990s. These new requirements roughly doubled the number of enrollees needed for an antibiotic clinical trial, making it prohibitively expensive and sometimes logistically impossible to successfully register a new antibacterial drug. The graph below tells the story.
The number of antibiotics approved per four-year window
A recent law, the 21st Century Cures Act, directs the FDA to facilitate the introduction of new antibiotics, but even if these changes are implemented it will be a couple of decades before the new drugs show up in pharmacies. However, the economics for inventing new antibiotic drugs are not expected to change. Estimated costs to develop a new anti-TB drug are $100 - $300 million, with attrition rates of more than 90%. It takes 250-500 patients treated with an antibiotic to see the same return on drug R&D investments as one person treated with a drug for a chronic condition. The market-return for antibiotics R&D is just not there. I might add, the first generation of antibiotics had safety issues that would never be acceptable to the FDA today. In fact, the FDA threw away eight effective quinolone antibiotics (cousins of Cipro) because of safety problems. They are throwing antibiotics away faster than we can create new ones.
There is much cheap talk and angst about this growing problem and its potential catastrophic consequences. However, until we get well down this path, not much is going to happen to address it. Our children may not be as lucky as Gregorio Zalles.
One final comment on the biological warfare use of bacteria. Bacteria, like viruses, are favorite infectious diseases among the BW jockeys. Anthrax is the easiest of all the infectious agents to weaponize. Japan tested anthrax on prisoners at its infamous Detachment 731 camp and subsequently developed a 40kg bomb, Ha, containing a mixture of shrapnel and anthrax spores. The US also established a biological weapons Manhattan-type project during the war which continued during most of the Cold War. The USSR had a massive BW development and deployment effort in that era. It is estimated that 100 pounds of weaponized anthrax spores dispersed upwind of a 500,000-person city has the potential to kill or disable half the city’s population. Anthrax spores field testing studies on Gruinard Island off the Scottish coast left the island uninhabitable for more than 50 years due to ongoing spore contamination. Cholera, typhoid, Salmonella, glanders and especially bubonic plague are favorites for obvious reasons. In fact, glanders was used by the Germans in their Mesopotamian campaign in WW1 to successfully infect 4500 mules.
From a casualty cost perspective, biological weapons are about $1/km2 versus $2000/ km2 for conventional weapons, which is very cost-effective warfare. As noted above with prions, it is now technically feasible to clone a potent toxin gene into a normally benign but highly communicable human gut or nasal bacterium, leading to a doomsday plague.



