
For the extremely obese (i.e., those with a BMI over 40), the most effective means of losing weight and keeping it off is bariatric surgery — as we have discussed in the past. Although some research has indicated that the effects of such surgery can be long-lasting, much of these data are derived from studies in which various types of bariatric surgery are used. A recent study, published in the New England Journal of Medicine, restricted its focus to people who had received the Roux-en-Y procedure (also referred to as Roux-en Y gastric bypass or RYGB).
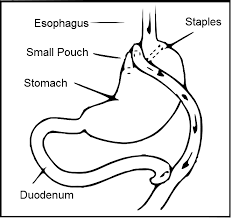
This type of bariatric surgery, as shown in the diagram below, involves restricting the stomach to a small pouch, and then attaching the distal end of the small intestine to that pouch. Thus food entering the stomach goes directly to the latter part of the small intestine, bypassing the first part where most nutrient absorption occurs.
The investigators, led by Dr. Ted D. Adams from Intermountain Healthcare in Salt Lake City, Utah, followed 418 patients who had RYGB surgery, and compared them to 417 patients who didn't have surgery (although they wanted to) because their insurance didn't cover it (non-surgery group 1 (NS1) and to a group of 321 equally obese people who didn't have surgery and hadn't tried to obtain it (NS2).
As expected, the surgery group lost more weight than either non-surgery group by 12 years post-procedure — - 35, three and zero percent respectively. In addition, the surgery group maintained an improved metabolic profile compared to either their baseline status or to the other groups. For example, their blood glucose levels dropped post-surgery, while those of NS1 and NS2 increased. Similarly, the level of LDL cholesterol decreased post-surgery while that of the NS groups had increased, and the opposite was true for HDL (good) cholesterol. Furthermore, the level of glycated hemoglobin (a measurement of glucose levels over time) didn't change in the surgical group, while it increased in both non-surgery groups. Also, of the 88 patients in the surgery group who had type 2 diabetes initially, 43 of those were no longer diabetic 12 years post surgery. By contrast, the risk of developing diabetes was less than one percent of that for either non-surgery group — a highly significant difference.
However, there was an association between bariatric surgery and death by suicide, an association that has been described in the past. The authors noted that it's unclear whether the increased suicide rate is related to the surgery itself, or might follow any large and sustained weight loss.
Thus, RYGB surgery seems to be successful for at least 12 years in terms of diabetes prevention or remission, as well as for improvement of lipid profiles and weight loss. The increase in suicide risk must be further explored.



