Understanding why there is an ever-increasing job dissatisfaction rate among doctors (see here) isn’t difficult to comprehend. Loss of autonomy, erosion of the ability to practice medicine (as expected and trained to do) and bureaucratic regulations that impede actual care (click here) top the list. Perverse incentives, ballooning of paperwork and physicians providing glorified data entry for electronic medical records need be included. Electronic medical records, pitched as panaceas, designed and vetted by user interface experts are at best a nuisance, at worst another obstacle keeping physicians from actually caring for their patients.
Isn’t disruption in an industry supposed to be for the better? Or, do I have it confused?
With all the emphasis on Big Data and its promised wisdom, what continues to astound me is how backwards that search has been. There is no greater wealth of knowledge or insight than the experienced practitioners on the front lines. Yet, the powers that be rarely, if ever, ask them about what the right data to pursue is or the problems that require solutions are – instead, the litany of solutions to problems we don’t have continues and gives birth to new and more problems.
Take a recent catastrophic medical emergency on a Jamaica-bound flight, for example. Two anesthesiologists on board identified a struggling woman and intervened upon her reported “complete respiratory arrest” (see article here). Limited by their circumstance and available equipment, they devised a makeshift ventilator to keep the passenger alive for roughly 45 minutes until an urgent landing could be made where she could be evacuated to a superior setting.
The wife of one of the physicians posted a more descriptive account on her facebook page:
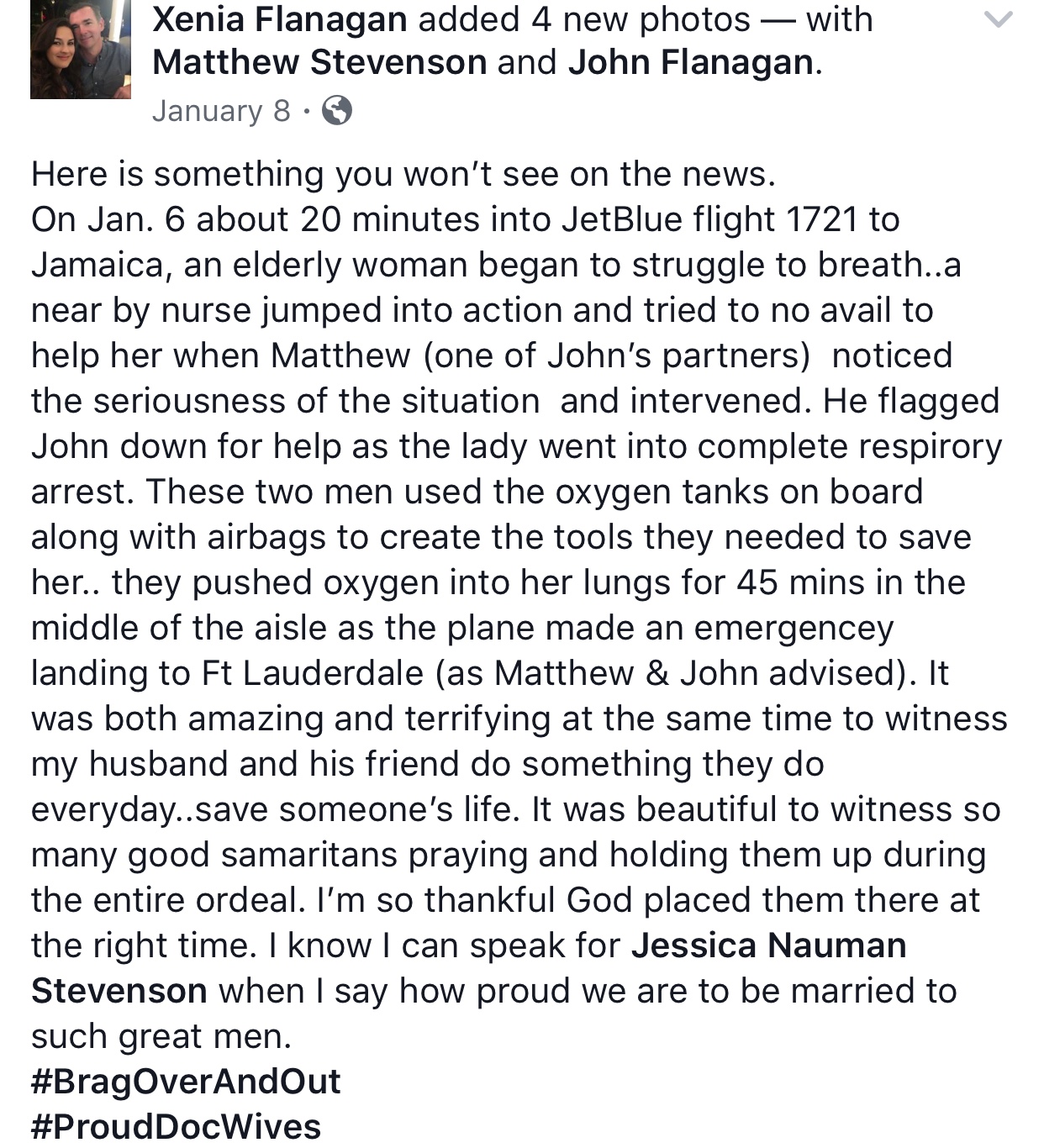

Doctors and health professionals continuously face shortages and are tasked to do more, often the heroic, with less and less. What motivates them is reducing suffering and long-term disability of another human being.
Numbers and data analysis cannot substitute for standing before an individual in anguish. Like firemen and police, physicians run toward the problems. These doctors worked with what they had, cutting tubing and air bags from emergency face masks from the ceiling.
Doctors are motivated by a need to serve the dis-eased. Extraneous actions that serve to redirect their attention to less meaningful matters fuels job dissatisfaction. Do you want to reinvigorate the legions of caregivers currently in the trenches? Find a way to increase the time we have to spend face to face with patients.
"Meaningfulness in this profession comes from one-on-one interactions with patients. The moment you feel like you're just another widget, it just takes the soul out of many physician's lives." - Abraham Verghese, MD
Why the combat terminology? Because practicing these days, sadly, is embattling the spirit of many who only ever wanted to practice medicine. Exalted billing platforms and unwieldy protocols imposed on physicians without their input has contributed substantially to the rise in “burnout.” As I have previously written, I don’t care for that designation as it serves to blame physicians for the ails of the health care system mostly caused by an endless pool of competing profit centers that marginalize patient and provider needs and wants.
I can’t remember the last hospital or office I worked in that had an actual tourniquet at the ready for blood draws or IV placement. You make do. You adapt. When a designated fancy warmer for a heel stick is unavailable, a diaper with warm water often does the trick.
When confronted by chaos, day in and day out, to varying degrees no matter the chosen discipline, it is quite extraordinary what scores of health professionals can design. They alone know what they and patients genuinely can and cannot live without in the medical realm.
Anonymous surveys with innate bias in the questions fail to amass the knowledge this brigade possesses. Open-ended forms and discussions would best serve that purpose. Speak to anyone in community health environments or those who trained at a Kings County Hospital in Brooklyn, for instance, where you do more in your first year of residency than rigid hierarchies in more academic centers will allow. The so-called industry experts, consultants, academic physicians with three months of clinical obligations annually can only be useful if they leave their offices and interact with those who don't position themselves to be medical "leaders."
Electronic medical records were supposed to reduce our burdens, allow us to speak with one another. Why is it 10 years after they were mandated that a whole new industry of scribes and interoperability (the buzz word for any computer program to talk to another) is developing? Another layer between physicians and patients.
Do you want to make health care better, ask physicians and nurses, the most experienced resources who at this point are being treated more as worker bee drones than the revolutionaries they might be meant to be.