Kidney failure results in the need for dialysis, to remove waste products, transplantation of a “new” kidney or death. All expensive options. Among the means to slow the onset of chronic kidney failure are dietary modifications, a recent paper points out that we have been remiss, for a variety of reasons, in recommending this helpful and low-cost measure. Perhaps it is time to more proactively recommend dietary “medicine.”
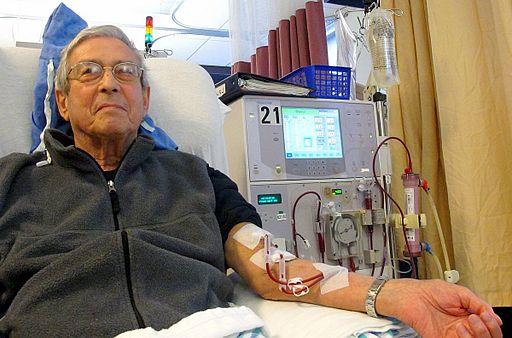
Kidney or renal failure is a progressive disease marked by an increasing inability to filter toxins from the blood and similar increased leakage of albumin, a type of protein, into the urine. It progresses through several stages and in its final end-stage, requires dialysis or transplantation. Most patients are identified in the intermediate phases, and the patient referred to a kidney specialist, the nephrologist for management. One of the recognized pillars of standard care is dietary interventions, to reduce the dietary burden of potassium (so no chocolate or bananas) or to find the right amount of protein that does not overwhelm the body’s ability to clear wastes and at the same time provides the necessary sources to manufacture the proteins used throughout our body.
Medical nutrition therapy (MNT) is a service authorized by Medicare for its beneficiaries with any degree of chronic renal failure or insufficiency. It is mandated for all patients on dialysis. While it has not been heavily researched the following will give you a sense of how often it is employed.
- In a study conducted 5-years after MNT as authorized for payment (2007) only 9% of 156,000 patients received care from a dietician before dialysis.
- In 2016, only 7,100 claims were filed with CMS for MNT despite a population at risk of 2.7 million
I am sure patients receive dietary injunctions from the nephrologists and are placed on diets restricting their fluid and protein intakes along with directives to avoid foods high in potassium and phosphorus. But does that reflect the “standard of care?” The answer here is unclear, because while the National Kidney Foundation recommends MNT, dietary guidelines in the presence of renal insufficiency have not been updated for 18 years.
MNT is different than having a brief conversation with a patient along with handing them a set of dietary instructions. MNT involves an assessment of the individual patient's diet and eating habits, and the patient’s subsequent nutritional behavior is monitored and reassessed. MNT is a form of dietary coaching, not just one and done. Medicare will pay for three visits during the first year of a patient having the diagnosis of renal insufficiency and for two visits annually after that. In rural areas, the service can be provided by telemedicine. And while it has not been studied explicitly in renal failure, it has proven cost-effective for both hypertension and diabetes, two common co-morbidities of renal insufficiency.
There are multiple causes for so few of these dietary evaluations. While dieticians may quibble about the $130 payment for the initial assessment, it is in line with physician payments for comparable services. More likely is the fact that only 48% of register dietitian nutritionists (RDN) are credentialed to provide services to Medicare beneficiaries and that many states do not recognize RDNs as Medicaid providers. Another unintended consequence of our payment structure is that a claim for MNT cannot be made on the same day as a claim for a physician office visit; the result, patients must return on another day wasting their time and increasing their transportation difficulties and costs.
There is no study showing MNT’s cost-effectiveness or that it is more effective than merely lecturing the patient and leaving them on their own. To be honest, for some patients, understanding medical directives is an uphill battle - they have problems with health literacy. But certainly it is a treatment worth pursuing, it has little cost and may provide a substantial benefit. In an atmosphere of rising concern over health care costs, this may be a useful preventative measure.
Source: Medical Nutrition Therapy for Patients with Non-Dialysis-Dependent Chronic Kidney Disease Journal of the Academy of Nutrition and Dietetics DOI: 10.1016/j.jand.2018.05.023