Like a preview reel at the movies, a new paper in Nature Medicine provides a teaser for how precision medicine might one day work; like all good previews, it raises many questions and leaves you wanting more.
It is an exploratory, proof of concept paper, no p-values or cost-benefit valuations. It is also a longitudinal study, mean participation closing in on three years, of 109 volunteers, whose physiology was evaluated every three months. By physiology, I am referring to the “omics,”
“…molecular profiling of the genome, gene expression (transcriptome), proteins (proteome), immune proteins (immunome), small molecules (metabolome) and gut microbes (microbiome), and wearable monitoring including continuous glucose monitoring.”
Glucose monitoring was included because the participants were “enriched” to include those at higher risk for diabetes. They found “67 major clinically actionable health discoveries,” from new-onset diabetes, unsuspected cancer, sleep apnea, a pathogenic cardiac mutation, to pharmacogenomic variations in how patients metabolize common cardiovascular medications like statins and warfarin. Carl Zimmer has written about the study in the New York Times and provides a good summary of their findings. I want, instead, to share my awe at the challenge that lies ahead.
We contain multitudes...
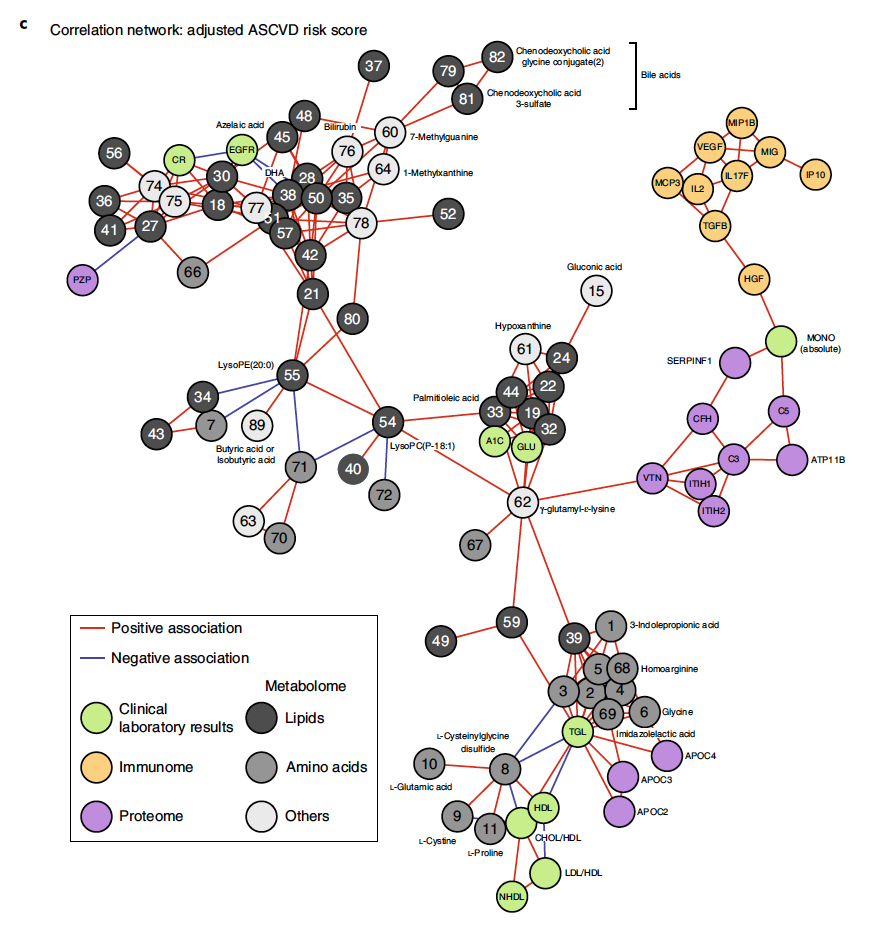
The graphic, taken from the paper, describes the network of findings that alter our risk of cardiovascular disease, positively and negatively. Those light green ones, the clinical laboratory results are the frequent targets of our medications, LDL, triglycerides, HgA1c, glucose. But the graphic is clear; those targets we currently treat are neither central nor controlling to the risk. One of the contributions of the study is to show the “omics” acting as a group and over time. The patients were evaluated quarterly so that, in returning to the movie metaphor, our image jumps and flickers badly, but it is beginning to be a better approximation of the involvement and interactions of so many factors over time. Given the intricacy of this dance of genes, environment and molecules, it is no wonder why some people look for the watchmaker behind the scenes.
With respect to diabetes, a specific interest of the study, “individual trajectory analysis revealed that participants followed multiple pathways to diabetes.” An elevated blood sugar, HgA1c, or oral glucose tolerance test is not necessarily definitive. Type 2 diabetes and increasingly now for Type 1 diabetes has more than one physiologic pathway, and the paths are not necessarily straight or in one direction. Much of what we measure, like HgA1c, are end-point summaries of many nuanced processes. For example, the researcher found HgA1c could alternate within the same individual between values considered normal, pre-diabetes, or diabetes – there was no linear progression from normal to abnormal.
The impact of the new knowledge
The participants were volunteers drawn from the Stanford area, making them highly educated, and given the time commitment, they were an extremely motivated group. So how did this new knowledge alter their behaviors? The graphic captures both the health discoveries and the changes in behavior.
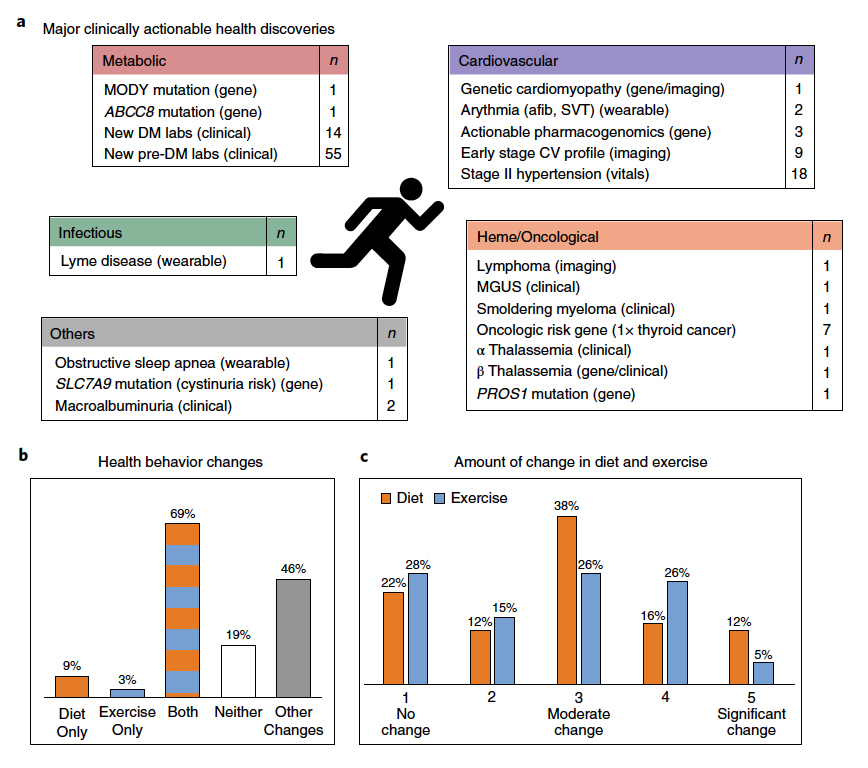
Many of the discoveries, like pre-diabetes, hypertension or early stage cardiovascular disease were identified by currently used clinical testing, just performed far more regularly and frequently than is current clinical practice. But in the case of the "pre-'s," it is unclear whether these patients will go on to develop these problems irrespective of what modifications we do or do not make.
Roughly 80% made changes in their lifestyles, more often to diet than exercise – no surprise there I suppose, it is easier to change what I eat than to spend several hours exerting myself. There were efforts to improve sleep, reduce stress, disconcertingly several participants increased their use of supplements, overall the patients became more self-aware.
The concern of many clinicians is that this type of additional information would provoke undue or unwarranted anxiety was not reported for these participants, at least directly. But 68% were concerned enough to discuss study results with their physicians, who in turn, affirmed or allayed their fears by ordering additional diagnostic testing in 29% of cases.
If you read Carl Zimmer’s article, take a minute to look at the comments. All of the usual memes are present, ranging from the views of the Luddites to New Age vibrations; these types of in-depth testing are unrealistic, they are too expensive, they heighten healthcare’s disparities based on income. Instead, for just a moment, reflect on the awesome beauty that is our physiology; appreciate how far we have come from the four elements of life to that diagram of cardiovascular disease risks, and recognize how much further we have to go on this journey. Precision medicine remains aspirational, but it is a glorious goal we have chosen to pursue.
Source: A longitudinal big data approach for precision medicine Nature Medicine DOI: 10.1038/s-41591-019-041406




