You got to love big numbers and what could concern us more than global death tolls; can you say “pandemic?” The World Health Organization tallies the global burden of disease (GBD) and has indicated that 70% is attributable to non-communicable diseases (NCD). Now a group of intrepid researchers, computer models, and a “growing database from epidemiological cohort studies” in hand have a focus on the deaths attributable to air pollution. Here is what the model shows:
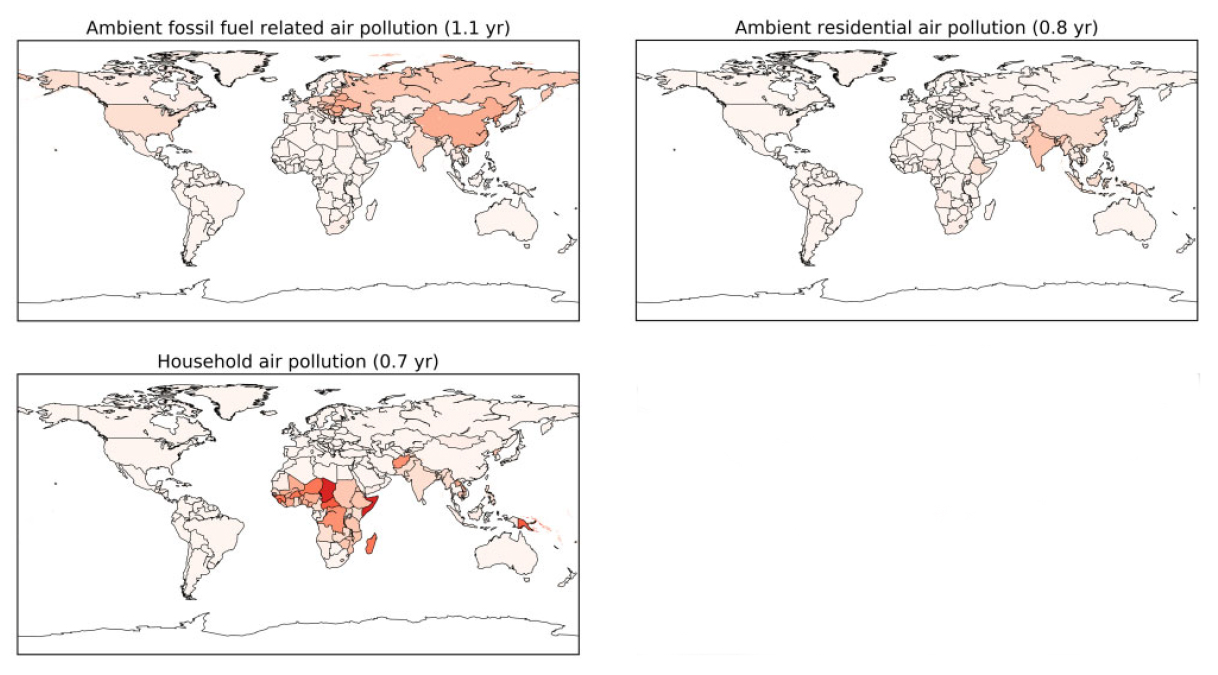
The darker the red, the greater the mortality. As we will shortly discover, the underlying numbers are quite fuzzy, but for a moment, let’s go with the flow, and take them as, at least, a consistent representation. The bulk of pollution’s mortality, two thirds, is in East and Southern Asia [1], especially the two economic powerhouses, China and India. For the America Firsters in the crowd, we trail at 4%, only South America and Australia have less. I was not able to find a clear definition of ambient residential air pollution, but I will assume that it is what we might call indoor air quality but that, of course, would include household air pollution, which is primarily from cooking, at least in the geographic areas of concern.
When looking at age, there is a bimodal distribution, with early child mortality, due primarily to lower respiratory tract infections, i.e., pneumonia. Again, there is a significant geographical disparity with the bulk of child mortality in Southern Asia, Africa, and Eastern Asia. The second age group at risk are those over 60 who have experienced longer exposures and whose deaths are primarily cardiovascular. The counterfactual here is that you might expect that air pollution would have a primary effect on the lungs. But respiratory disease, lower respiratory tract infections, COPD, and lung cancer account for only 30% of global mortality attributable to air pollution; half is due to cardiovascular disease, and the remaining 23% is due to diabetes, hypertension, smoking, and elevated cholesterol.
The short-hand for it all is that low and middle-income countries have both large populations and significant sources of air pollution from fossil fuel use to the use of coal or biomass for cooking. They also have, and I will be the first to admit that I am painting with a broad brush, sub-optimal health systems. So, while air pollution may well play a role in our health, so do the unmeasured health systems.
The researchers used a number of metrics to make their point in addition to mortality. They included a measure of years of life lost as well as the number of years of avoidable loss. The years of lost life varied from a high of 3.9 years in East Asia, to a low of about 9 months in Australia. The researchers determined the avoidable loss of life expectancy by removing all the avoidable pollutants, fossil fuels, biomass used for cooking, and various agriculture pollutants like NH3 from the model. With the exception of Africa and Australia, this would reduce the loss of life years by between 50 and 75%. Of course, they did not calculate the loss of life that might be attributed to such a massive loss of energy to the world through hunger, thirst and the associated rioting.
Fuzzy numbers
There are many assumptions and estimates within the model. As to the attributions of mortality, and that is the meat in this paper, there are wide confidence intervals; the data is limited by the number of countries whose data was actually used and subsequently extrapolated. The PM2.5 data does not take into account its source which may make it more or less toxic. And while they assure us that the “exposure calculations contribute relatively little to uncertainty,” that is only because they are overshadowed by the attribution data’s uncertainty. And exposure calculations, especially of residential/household air pollutants remain problematic.
What we can safely conclude is that whatever excess mortality may be attributable to air pollution, that mortality involves specific geographic areas with large low and middle-income populations that do not have the benefit of high-income health systems. No one can argue against cleaner air, but to continue increasingly tighter limits on pollutants, while ignoring the need to improve health care and shift cultural norms with respect to smoking and cooking fuels is too limiting an approach.
[1] Southern Asia - Afghanistan, Bangladesh, Bhutan, Maldives, Nepal, India, Pakistan, and Sri Lanka. Eastern Asia - Japan, North Korea, South Korea, Mainland China, Taiwan, Hong Kong, Mongolia, and Macau West Asia - Afghanistan, Armenia, Azerbaijan, Bahrain, Cyprus, Gaza Strip, Georgia, Iran (Islamic Republic of), Iraq, Israel, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, Syrian Arab Republic, Turkey, United Arab Emirates, West Bank, and Yemen
Source: Loss of life expectancy from air pollution compared to other risk factors: a worldwide perspective European Society of Cardiology DOI: 10.1093/cvr/cvaa025