Last winter, extending into the early spring, the treatment for COVID-19 was at best ill-defined. All of our treatment protocols seemed ineffective, and healthcare teams tried everything under the sun to save lives. A new study looks at whether all of our experimentation has yielded improved care – spoiler alert; the answer is yes.
There are two ready explanations for why care may have improved, physicians got better at treating the disease, or the patients contracting COVID-19 were not as frail – younger, with fewer co-morbidities, you know, those “Spring-break” kind of cases. The study sought to answer which hypothesis was more likely. It is retrospective, based upon England’s COVID-19 critical care hospitalizations, 21,000 patients. Pregnant women were excluded. The patients all required either ICU care or “high dependency” units (HDU); what we would term in the US, “step-down” care, patients being closely monitored but without the need for full life support, e.g., ventilators and some intravenous medications meant to stabilize blood pressure.
Results
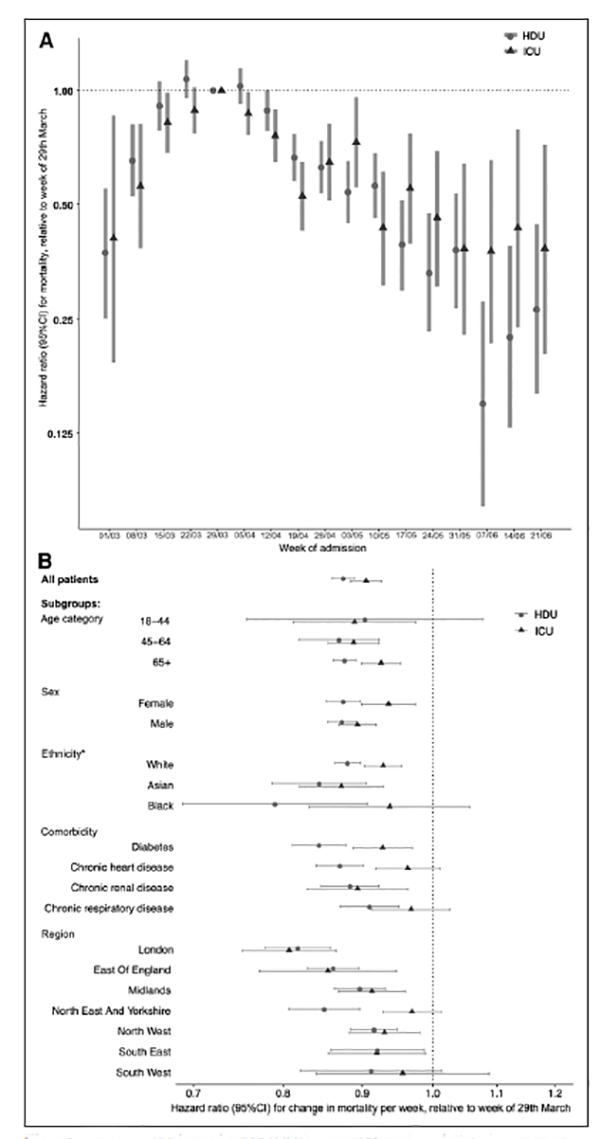
Of the 5,715 patients in the ICU, 35.8% died; of 15,367 patients in HDU, 22.3% died between March and the end of June
Unadjusted survival was lowest in both units at the beginning of the study. The chart to the left summarizes the key findings.
- The good news, survival improved for every age, gender, ethnicity, “and in people with major co-morbidities” in both the ICU and HDU settings.
- The bad news, the improvement was good, not great - roughly 13% in HDU, 9% in ICU.
There were some geographic variations in the degree of improvement, consistent with varying patient populations and treatment protocols.
But the bottom line is that outcomes improved as physicians, and the rest of the healthcare teams got more experience in treating COVID-19. And this is long before we began to use remdesivir or steroids on a protocol-driven basis; this was in the kitchen-sink days of treatment protocols. The researchers report that some of these patients did receive dexamethasone and remdesivir, so the study does not tell us whether our pharmaceutical management is to obtain more credit than our non-pharmacologic interventions. The study is also limited in that all the relevant outcomes may not have been fully reported when the analysis was done.
Source: Improving Survival of Critical Care Patients with Coronavirus Disease 2019 in England Critical Care Medicine DOI: 10.1097/CCM.000000000004747