Hospitals billed for care based on International Classification of Disease (ICD-10) codes, and early in the pandemic, there was no specific code for COVID-19. That changed on April 1st when a need code was issued specifically for this disease - U07.1 for the obsessed. Previously the CDC recommended coding the clinical problem, usually pneumonia, to be appended with "other coronavirus as the cause of diseases classified elsewhere." The researchers used a database containing a 20% sample of all hospitalization in the US from January 1st to May 31st. They cross-referenced those discharge codes with another dataset containing PCR test results on the same patients. Here is what they found:
- Of 3,128,064 inpatient discharge records, roughly 82,000 recorded COVID-19 (2.65%)
- About 74,000 used the new code, 8,600 the older, legacy code
- Hospitals rapidly switched to the new code within two weeks of its introduction
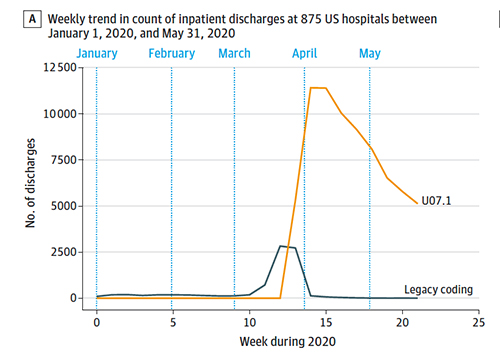 There is a long history of studying the diffusion of innovation. In medicine, the diffusion often occurs over years. A shift over two-weeks is remarkable. Of course, that coding shift results in potentially higher payments to the hospitals, so you may expect it to be incentivized!
There is a long history of studying the diffusion of innovation. In medicine, the diffusion often occurs over years. A shift over two-weeks is remarkable. Of course, that coding shift results in potentially higher payments to the hospitals, so you may expect it to be incentivized!
The researchers go on to correlate the finding of PCR testing for COVID-19 with hospital coding. They identified 52,000 results to associate with those hospitalizations. They found that in the presence of a positive PCR, the hospitals coded for COVID-19 92% of the time. In the absence of a positive PCR result, hospitals coded for COVID-19 0.21% of the time. In short, hospitals reliably coded for U07.1, COVID-19. The authors conclude
"The findings suggest that hospitals appear to provide reasonably accurate COVID-19 diagnosis codes in administrative data, and these codes may be a reasonable means to track inpatient discharges and costs associated with COVID-19."
Do you agree? Discuss among yourselves.
Did you note the misdirection? Upon closer reading, notice that PCR results were available for only 52,000 of the 74,000 hospitalizations that used the new code. Twenty-two thousand discharges had no microbiologic evidence to support their coding. Let us not rush to infer intent; after all, only The Shadow knows "what lurks in the minds of men."
But we certainly can say that those additional cases, nearly 30%, without confirmatory evidence, make the data uncertain. Coding is based upon the treating and consulting physicians' written notes as abstracted by hospital-employed "coders." I've worked with them over my clinical career. They are dogged in getting the documentation they need to fit into an accepted category and consistently do not try to influence the physician's judgment.
COVID-19, just like Toto, that little dog, has once again pulled back the curtain and asked us to "Pay no attention to that man behind the curtain!" The dataset on COVID-19, like those for heart disease, diabetes, and all the others, is not entirely correct. It is our best work currently and, as with all human endeavors, can be improved. Fighting about the accuracy of these numbers gives them objectivity they do not deserve. Take them as our best effort, learn what you can, and move on.
Source: Uptake and accuracy of the Diagnosis Code for COVID-19 among US Hospitalizations JAMA DOI: 10.1001/jama.2020.20323




