Evidence confirming the relative safety of vaping continues to build. Multiple studies have now clearly shown that e-cigarette use is far safer than traditional smoking and effective in helping many people give up combustible cigarettes. But what about the secondhand impacts of vaping? A study just published in BMJ Thorax claims that “Secondhand nicotine vape exposure” may be associated with increased risk of bronchitic symptoms and shortness of breath in young adults. The authors concluded that their
"… results have important public health implications for the population exposed to secondhand nicotine vape. Unlike active vaping and smoking, secondhand nicotine vape exposure is not a voluntary exposure. Therefore, if the associations we observed are causal, prohibiting e-cigarette use in public places is warranted, just as secondhand tobacco smoke exposure has been prohibited in public spaces for decades ...”
A careful reading of the paper indicates that this is little more than wishful thinking. The possibility that vaping has serious secondhand effects is speculative at best and offers little justification for restricting vaping in public places.
A look at the study
The researchers surveyed 2,097 high-school students who self-reported their secondhand vapor exposure and health data in four waves between 2014 and 2019. There were 2,090 participants in wave 1 in 2014; 1,609 in wave 2 the following year; 1,502 in wave 3 in 2017; and 1,637 in wave 4, about 78 percent of the original sample, in 2019. Twenty-three percent of the original students (481 participants) dropped from the study at wave 2 after graduating high school. There was a relatively small association between secondhand vapor and the reported respiratory systems.
Over the study period, an increase in the prevalence of wheeze and bronchitic symptoms was observed in the study population (not statistically significant). The prevalence increased from 12.3% to 14.9% for wheeze and 19.4% to 26.0% for bronchitic symptoms (figure 2). The prevalence of shortness of breath did not show any clear trend over time, with prevalence of 16.5% in wave 2, 18.1% in wave 3 and 17% in wave 4.
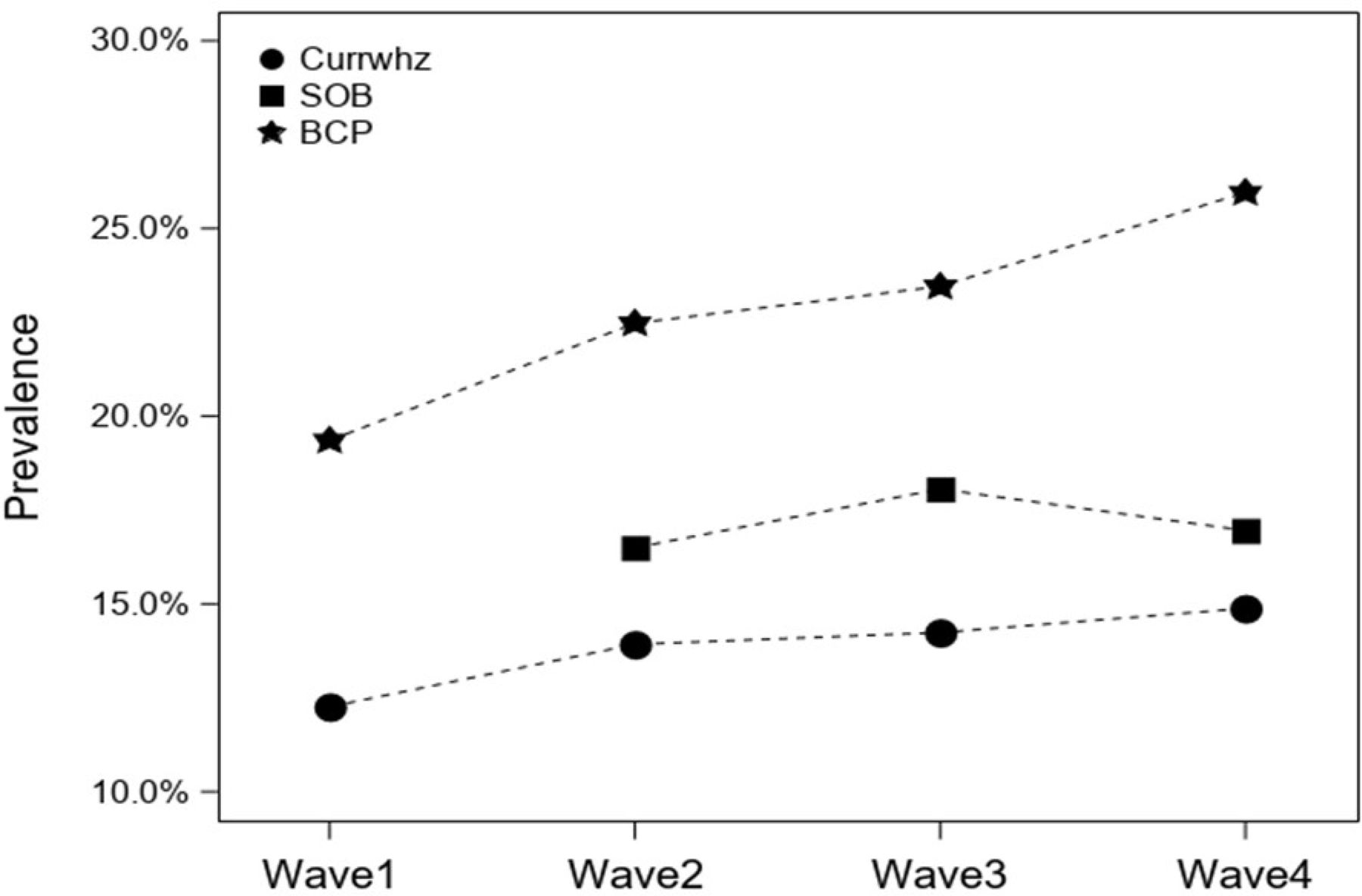
Figure 2: Prevalence of wheeze, bronchitic symptoms (BCP) and shortness of breath (SOB) during the study period (waves 1–4). BCP, Bronchitic symptoms reported in previous 12 months; Currwhz, wheeze reported in 12 months; SOB, shortness of breath reported in previous 12 months.
Important limitations
The study is a first step toward more comprehensive research about secondhand vaping, but its significance was restricted by a number of crucial limitations, which, to their credit, the authors acknowledged. The first major problem was this:
A majority of the participants (76.0%–93.1%) who had secondhand nicotine vape exposure during any of the study waves was also likely to have personal use of tobacco or cannabis products or secondhand exposure to combustible products
The researchers reported that disentangling the effects of secondhand vapor from those of tobacco and cannabis, which are also linked to respiratory distress, was “challenging,” though they were able to adjust for these confounders in their models. But, frankly, I'm not sure they succeeded.
Exactly how do you determine if someone's respiratory symptoms were due to secondhand vaping without knowing how much nicotine vapor or cannabis smoke they were exposed to, or how often they were exposed? Asking them if anyone in their household vapes or uses cannabis tells you next to nothing.
The researchers similarly measured active smoking and vaping during the previous 30 days with a single yes/no question. This metric would include someone like me, who vapes multiple times every day of the week, and someone who vapes just once a month. Those are significantly different exposures that the researchers defined as identical. Additionally, as reported in supplemental table E2, only “542 study participants reported secondhand nicotine vape exposure during the study period,” meaning only a minority of people in the study actually had the exposure of interest.
And, of course, the researchers were entirely dependent on high-school students to accurately report their exposure to nicotine vapor, tobacco, and cannabis, as well as their related health outcomes at each wave. Recalling what my friends and I were like at 17, that sounds like a fool's errand—as does using a study like this to guide public policy.




