About a week ago, news outlets reported that a large randomized controlled trial showed that ivermectin had no impact on COVID. At that time, only scant data on which the conclusions were based were available; the actual paper wasn't available.
Since then, "Effect of Early Treatment with Ivermectin among Patients with Covid-19" has been published in NEJM, and the data are now available. Below I've carved up and analyzed some key data tables from which the conclusion was reached. (The TOGETHER trial (1) was conducted in Minas Gerais, a state in Brazil.)
Let's take a look at the data that led the authors to this conclusion. First, we need to examine how the trial was set up and what was measured.
1. Baseline characteristics
Table 1 is a truncated version of the paper's full table of 20 baseline characteristics, e.g., BMI or asthma, which were used to match the ivermectin and placebo groups (679 participants each). The close match between the percentages in the ivermectin (blue boxes) and placebo (red boxes) groups shows that there is a good balance between the two groups, making selection bias unlikely.
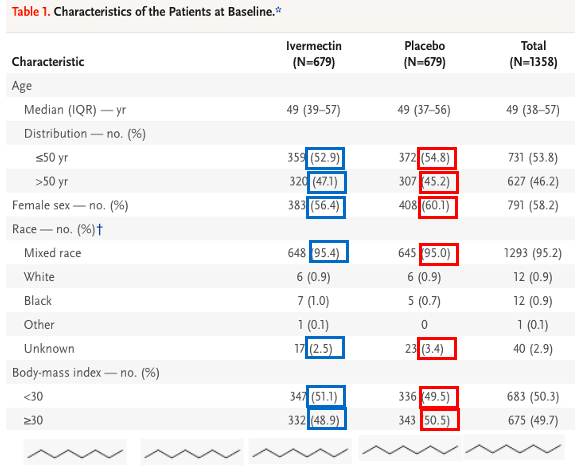
Table 1. Selected baseline characteristics of participants in the TOGETHER trial. Source: NEJM
2. Randomization
The TOGETHER trial was randomized and double-blinded. This required that neither the patients nor the medical staff were aware of who was in each group, how they were assigned, or which patients received drugs or placebo. (Emphasis added)
Patients underwent randomization by means of a block randomization procedure for each participating site, with stratification according to age (≤50 years or >50 years). The trial team, site staff, and patients were unaware of the randomized assignments. The active drug and placebo pills were packaged in identically shaped bottles and labeled with alphabetic letters corresponding to ivermectin or placebo... Only the pharmacist who was responsible for randomization was aware
Results
Randomized clinical trials – the gold standard of clinical trials, must have a primary outcome (often several of them) determined in advance when the trial protocol is established. Prospective trials, like this one, ask questions and then collect data to get answers. Retrospective trials, which are inferior, analyze past data and look for answers or trends. One of the knocks on retrospective trials is that the conclusions can differ depending on what data is selected for analysis (selection bias).
In the Brazilian trial, the primary outcome was whether people, all of whom had confirmed COVID infections, were either hospitalized due to COVID or became sick enough from the infection to require a visit to an emergency room within 28 days.
All participants received a placebo or ivermectin once a day for three days (the ivermectin dose was 400 micrograms per kilo bodyweight – about 28 milligrams). In the ivermectin-treated group (blue box), 100/679 (14,7%) of the patients who received the drug (blue box) were later hospitalized or sought ER treatment, while 111/679 (16.3%) of people in the control group (red box) met the same criteria. The relative risk (RR, 0.90, yellow arrow) is not statically significant. In other words, there is no difference between 14.7% and 16.3%. The number of people who met the criteria of the primary outcome was the same in both groups.
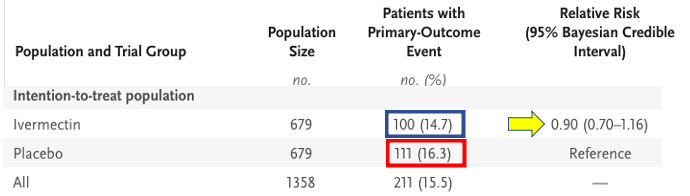
Table 2. Primary outcomes for placebo and ivermectin treated participants. The percentage of patients with a primary outcome event was the same in both groups. The RR (0.90) also indicates this.
The data, broken down into sub-groups, can be visualized in a Forest plot. In short, when the horizontal line crosses the vertical (1.00, RR line, the range of the data), it means that there are no differences between the ivermectin group being better (to the left, red box) or the placebo group being better (to the right, blue box). All data lines cross the vertical line; there is no difference between drug and placebo in any of these sub-groups, regardless of the participants' baseline characteristics.
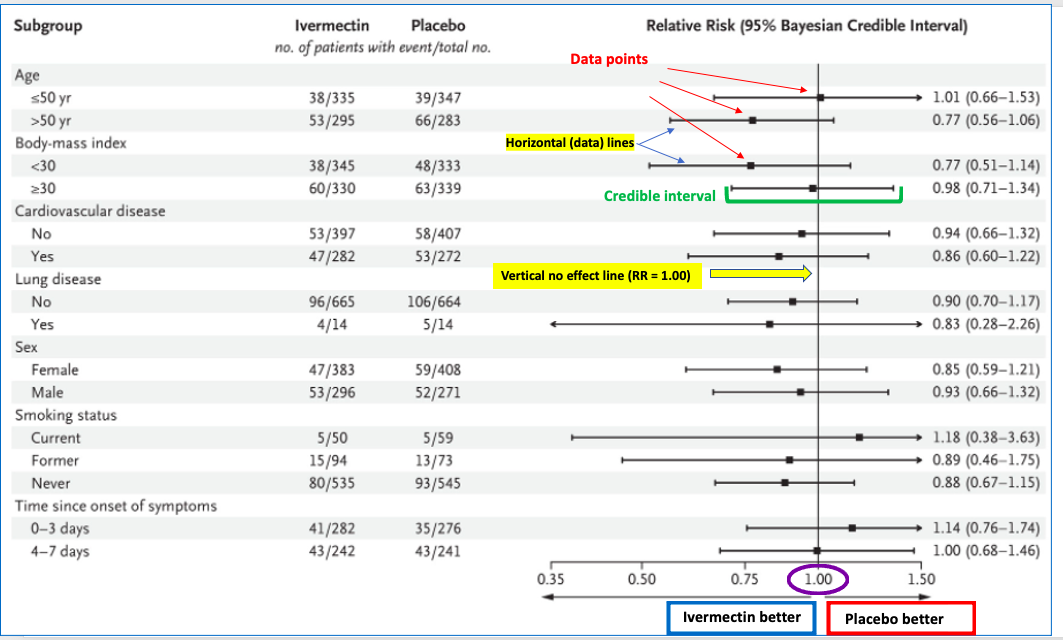
Table 3. Forest plot of subgroups of COVID patients.
3. Secondary Outcomes
Numerous other parameters were measured. The truncated table below shows no statistically significant differences between the ivermectin and placebo groups, including viral clearance, number of days in the hospital, number of days on a ventilator, and others. The complete data table for secondary outcomes can be found here.
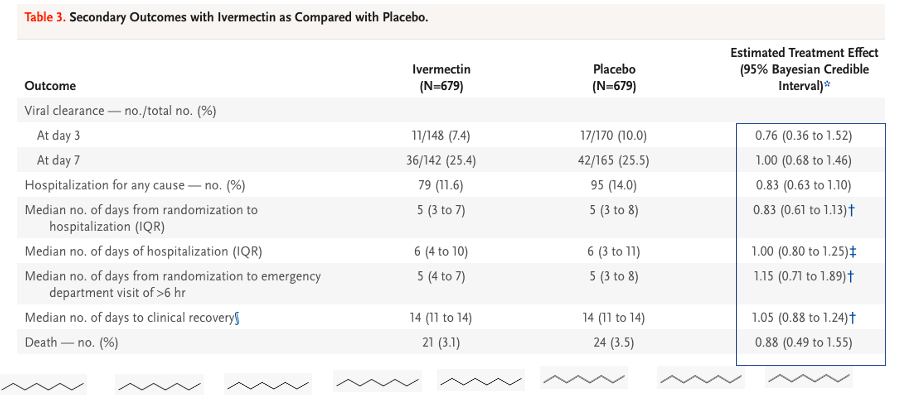
Table 4. Secondary outcomes comparing ivermectin and placebo (truncated).
Table 4 is quite large making the data hard to see, even when truncated. I selected five important secondary outcomes and entered the data into excel:
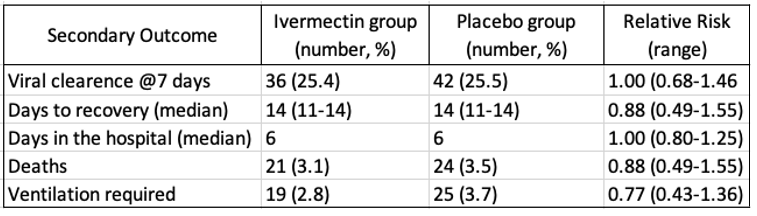
Table 5. Selected secondary outcomes.
4. Conclusion
Treatment with ivermectin did not result in a lower incidence of medical admission to a hospital due to progression of Covid-19 or of prolonged emergency department observation among outpatients with an early diagnosis of Covid-19.
E.J. Mills, et. al., New England Journal of Medicine, March 30, 2022
DOI: 10.1056/NEJMoa2115869
5. What this study does and does not show
It is impossible to prove a negative, so the TOGETHER trial cannot prove that ivermectin is not useful in treating COVID. But the study provides solid evidence that ivermectin is no better than a placebo when given at a dose of roughly 30 milligrams per day over a three-day interval. Other groups will most likely conduct other RCTs, perhaps using ivermectin at different doses, different intervals of treatment, or in combination with other drugs.
6. Impression
When comparing the efficacy data in this study with that for Paxlovid (or even molnupiravir), the difference is stark. Paxlovid and molnupiravir, both direct-acting antiviral drugs, clearly show clinical utility against COVID by well-established mechanisms that have proven successful in inhibiting other viruses like hepatitis C, herpes, and HIV/AIDS. It is difficult to see how tweaking the dose, length of treatment, or adding additional components would make enough of a difference to give ivermectin a place on pharmacy shelves next to current therapies.
NOTE:
(1) The TOGETHER Trial (actually a series of trials) are randomized clinical trials conducted to investigate the efficacy of repurposed treatments for SARS-CoV-2 infection among high-risk adult outpatients. Other TOGETHER trials have examined different drugs, for example, lopinavir and hydroxychloroquine, which are used for HIV infection and malaria, respectively.




