A recent, scary article in the Boston Globe proclaimed the following:
"A puzzling phenomenon: Patients report a rebound of
COVID-19 symptoms after taking the antiviral Paxlovid."
Uh oh. We finally caught a break when Pfizer's Paxlovid, a combination of ritonavir and nirmatrelvir (1), was shown to be remarkably effective in reducing hospitalization and deaths from COVID. And it wasn't just a break; it was a breakthrough – an effective medication in pill form that can be taken following a positive COVID test and have a profound effect on the course of the disease.
“I think it is the beginning of a ‘game-changer'...It's really our first efficacious oral antiviral pill for this virus. It shows clear benefit, and it really can prevent hospitalization and death in people who are at high risk.”
Scott Roberts, MD, a Yale Medicine infectious diseases specialist.
What's with the headline? Is Paxlovid, the only drug that has taken a big chunk of fear out of COVID, starting to fail? Kathy Lazar, writing for the Boston Globe (at the very least), insinuates this.
"And it’s not just their symptoms that reappear. Many report that after finishing their five-day course of treatment, feeling better, and testing negative on an at-home rapid test, they then test positive again a few days later."
Kathy Lazar, Boston Globe 4/21/22
I'll save you the time of checking her "links," such as they are. The first is a tweet from one doctor, and the second is a Reddit discussion where a single person describes their experience, and several others chime in. I'll leave it to you to determine whether the allegedly high journalistic standards of the Globe are met here.
To be fair, Lazar asks the right questions:
The issue has captured the attention of at least two teams of Boston-area scientists, who are trying to understand what might be fueling the problem. Resistance to the drug? Patients being quickly reinfected? Or maybe some people just need to take the medicine longer to mount a more effective immune response.
Let's examine the possibilities.
1. Resistance to drug
Protease inhibitors (PIs) are not new; they have an impressive successful track record (2). Saquinavir, arguably, one of the most important discoveries in the history of pharmaceutical research, was launched by Roche in 1995, marking the first time in the 14-year history of AIDS in the US that deaths began to decline. PIs, along with nucleoside drugs, later formed the basis of the AIDS cocktails, which have transformed the infection from a certain death sentence into a chronic, manageable disease. Invirase and the dozen or so PIs that followed it saved many lives. PIs work.
As I have written, the mechanism by which Paxlovid inhibits the virus (at least so far) is independent of the variants with multiple mutations in the viral spikes. At this time, I am unaware of any of the thousands of sequenced variants that show resistance to Paxlovid. Neither are the authors of a 2022 review in the International Journal of Molecular Sciences:
Currently, data are available only for the circulating natural variants of SARS-CoV-2 Mpro, and PI-resistant variants have not been identified to date although multiple studies were conducted for the identification of those residues of SARS-CoV and SARS-CoV-2 PRs that may confer to drug resistance.
J. Tozsér, et. at. 'Potential Resistance of SARS-CoV-2 Main Protease (Mpro) against Protease Inhibitors: Lessons Learned from HIV-1 Protease.' Int. J. Mol. Sci. 2022, 23, 3507. https://doi.org/10.3390/ ijms23073507
Conclusion: Based on Paxlovid 's mechanism of action and the absence of documented resistance to the drug, this is probably not the correct explanation of the reported cases of COVID rebound.
2. Patients Being Quickly Reinfected
This one makes no sense. Although some people have caught COVID more than once, especially when Omicron made its appearance, people who took Paxlovid felt better and then suffered a "second" episode shortly thereafter don't fit the bill as being reinfected.
A reinfection is when a person becomes infected with COVID, enough time passes, and later becomes infected again. A person is considered to have been reinfected if they test positive again 90 days or more after their first positive test.
The following from CDC further casts doubt on the reinfection theory : (my emphasis)
Multiple studies have compared the incidence of reinfection... during a specific time period to evaluate the level and duration of protection provided by initial infection with SARS-CoV-2... data from seven observational cohort studies assess[ed] the risk of reinfection over time. In these studies, primary RT-PCR-confirmed SARS-CoV-2 infection decreased [the] risk of subsequent infection by 80–93% for at least 6–9 months...
CDC, 'Science Brief: SARS-CoV-2 Infection-induced and Vaccine-induced Immunity' 10/21
Conclusion: People who suffered rebound COVID a few days after Paxlovid therapy probably did not become ill (again) because of reinfection.
3. Insufficient dose or treatment time
How long does it take to clear SARS-CoV-2 from your body? Ironically, the best answer to this question comes from the TOGETHER randomized controlled trial that examined the effect of ivermectin vs. placebo on multiple parameters of COVID, one of which was the number of days it took to clear the virus (Figure 1).
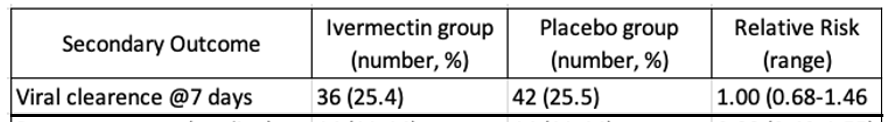
Figure 1. Only 25% of the participants cleared the virus after 7 days in both the ivermectin and placebo groups.
In other words, if only 25% of the trial participants were able to clear the virus with no treatment, the time to achieve complete viral clearance must be considerably longer, perhaps 2-3 weeks, maybe more. How long does it take for patients treated with Paxlovid to clear the virus? While this precise information is not available from Pfizer's clinical trials, the company does report the following:
An approximate 10-fold decrease in viral load at Day 5, relative to placebo, was observed in both EPIC-HR and EPIC-SR, indicating robust activity against SARS-CoV-2 and representing the strongest viral load reduction reported to date for a COVID-19 oral antiviral agent
This gives us a solid clue about what's really going on. While a five-day course of Paxlovid is sufficient to keep ~90% of COVID victims out of the hospital and reduce their viral load 10-fold, there may be a subpopulation of people who either didn't respond as well as others to Paxlovid or, perhaps, had a higher viral load, to begin with. Of the three theories proposed in the Globe article, this one makes the most sense, probably by a lot.
4. What to do?
It is far from clear that there is a problem at all. The Globe article fails to report how many people have suffered from COVID rebound. The story is anecdotal and probably sensationalistic. If COVID rebound following Paxlovid is a real issue, then perhaps a longer course of treatment may be a simple solution, just like a two-week course of antibiotics might be required to treat an infection when a one-week course is insufficient.
5. Bottom line
There doesn't seem to be much to worry about at this time.
NOTES:
(1) Paxlovid is a two-drug combination of nirmatrelvir, the antiviral agent, and ritonavir, which slows the metabolism of the nirmatrelvir, keeping the concentration in the blood at a sufficient concentration to beat back the virus.
(2) Two protease inhibitors were developed to combat hepatitis C. Boceprevir and telaprevir were the first two direct-acting antiviral drugs developed against HCV.




