The air pollution epidemiology literature includes morbidity studies involving specific indoor exposures such as smoking or gas cooking, but comprehensive studies contrasting indoor with outdoor environments are lacking. [1] The EPA Office of Indoor Air Quality issues guidance and recommendations as if outdoor air were pristine, and EPA epidemiology-based risk assessments assume that we all live outdoors. Considering indoor environments is not an idle pursuit.
The Problem
This conflict between outdoor and indoor pollutants was highlighted during the COVID pandemic by the CDC’s recommendation to increase residential ventilation by outdoor air with no particular regard for the quality of that air. The CDC apparently has no problem with increasing exposures for compromised patients to the same polluted air that EPA risk assessments claim to be lethal at any concentration. So, which is it? Is outside air beneficial, or can it be deadly? How are we supposed to know?
What do we know about “exposure” to outdoor air pollution?
- Public-use data are limited to what is collected for compliance with air quality standards. Unregulated “pollutants” are not routinely monitored, nor are background levels or contributions from local sources like traffic.
- Historical data or cumulative exposures have seldom been used to study chronic health effects.
- Concentration levels are sensitive to atmospheric conditions (temperature, wind speed).
- Epidemiology studies have either been based on data from the nearest routine monitor or on mathematical models of increasing complexity but limited validation.
What do we know about “exposure” to indoor air pollution?
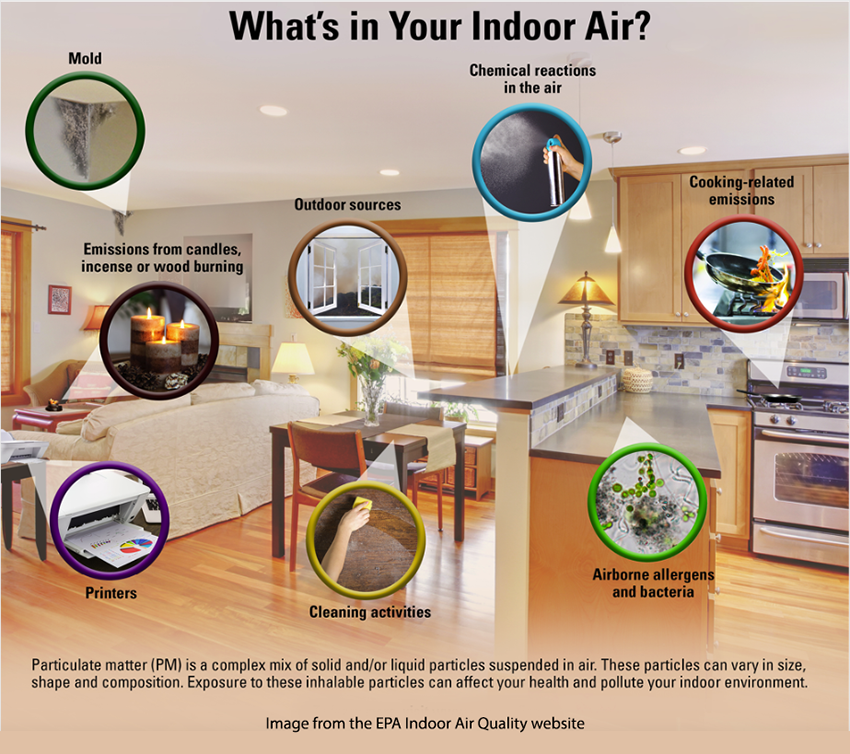
- Indoor air quality depends on the types and usage of indoor pollution sources, infiltration of outside air, ventilation within the building, and adsorption onto and reactions with interior surfaces, e.g., the residual tobacco odor on furniture or draperies from smoking.
- Without interior ventilation, air pollution from quasi-continuous indoor sources such as cooking could reach high concentrations. The buildup of large-particle dust on horizontal surfaces is such a cumulative effect.
- By contrast, reactive gaseous pollutants such as ozone or sulfur dioxide (SO2) are unlikely to accumulate indoors. With the possible exception of photocopy machines, there are no indoor sources of ozone.
- Interior ventilation is characterized by the number of air changes per hour (ACH) which will vary with how “tight” the construction is; newer homes, for energy efficiency, do not have as high an ACH as older construction.
- As a result of these and other factors, Indoor exposures may vary greatly from house to house within the catchment area of an outdoor monitor; outdoor air quality cannot represent personal exposures.
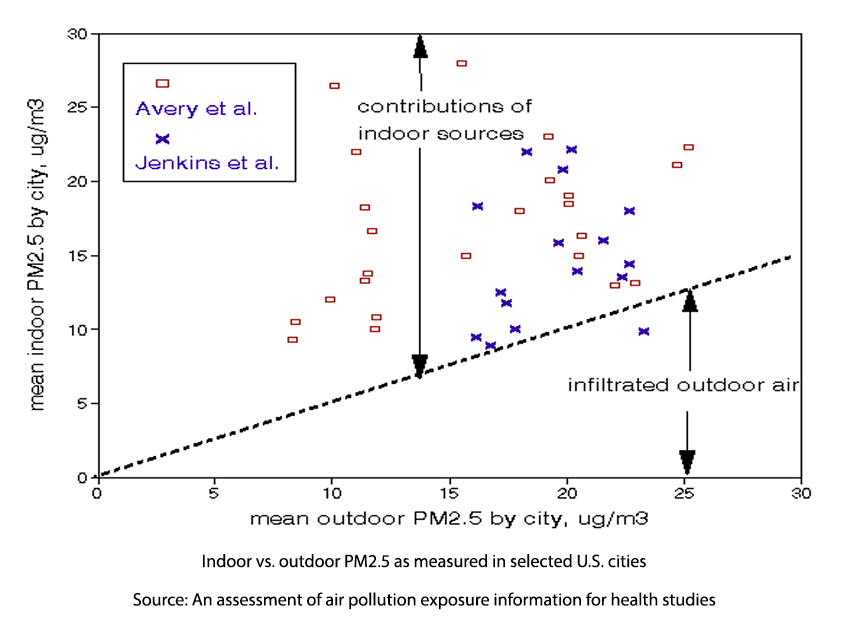 The graph compares indoor and outdoor PM2.5 data from two groups of cities. There are no relationships between indoor and outdoor concentrations. Indoor levels are less than about half of the corresponding outdoor level. If an epidemiological study had been based on 12 µg/m3, personal exposures could have ranged between 10 to 28 µg/m3.
The graph compares indoor and outdoor PM2.5 data from two groups of cities. There are no relationships between indoor and outdoor concentrations. Indoor levels are less than about half of the corresponding outdoor level. If an epidemiological study had been based on 12 µg/m3, personal exposures could have ranged between 10 to 28 µg/m3.
Our Homes - chemical reaction chambers.
Indoor environments differ in important ways. First, emissions are not dispersed by outdoor weather patterns; what’s emitted indoors tends to stay there, becoming ever more concentrated unless diluted by infiltrating outdoor air and modified by physical and chemical reactions with interior surfaces. A building can protect occupants against reactive species like ozone, SO2, or acidic particle while adding pollution exposures from combustion, furniture, or construction materials.
Infiltration of outdoor air, characterized by the air exchange rate (ACH), is required to maintain a healthy indoor environment; Inflows of outdoor air must be balanced by equivalent outflows of mixed air. As a result of this process, indoor pollutant concentrations will differ from outdoor levels, in some instances becoming more and, in other cases, less concentrated. Consider passive smoking. In the absence of infiltrating outdoor air, indoor PM2.5 levels could reach those of the exhalations of the smoker. Still, experiments have shown that steady-state indoor levels are not that but, but often 2-3 times outdoor ambient levels.
Air Exchange Rates
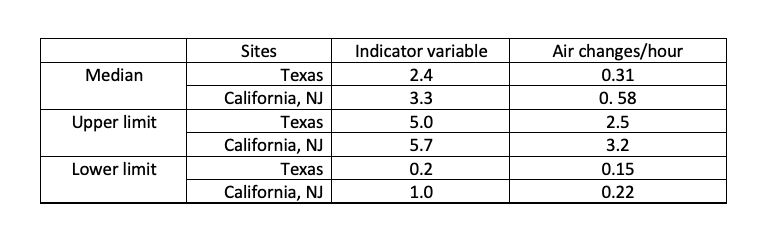
The air exchange rate ACH, which will depend on windows, use of exhaust fans, construction tightness, and building age; outdoor wind conditions may also be important. Building codes may specify minimum ACH design values, but actual field data are sparse. The graph shows ACH frequency distributions found in 3 U.S. locations [2].
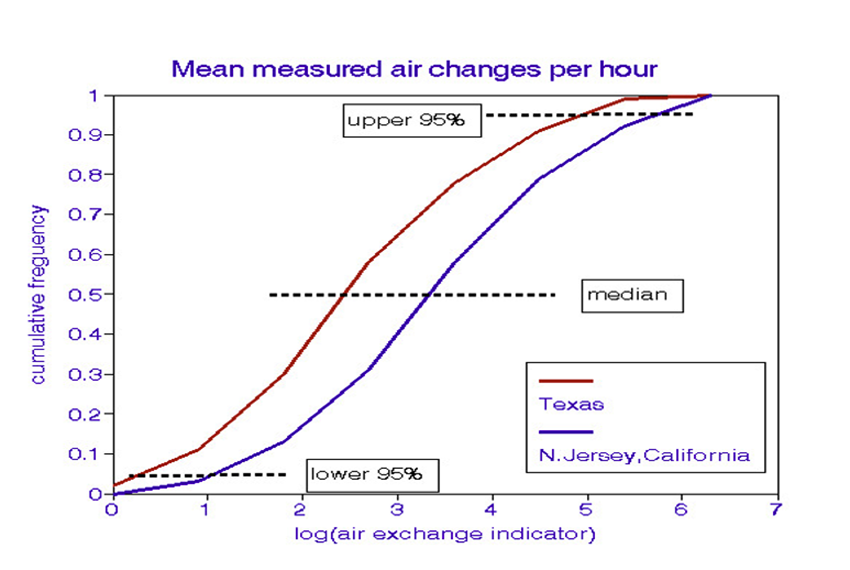
The distributions are shown here in terms of an ACH “indicator variable” A wide range in ACH values and indoor-outdoor air quality relationships should be expected in community-wide relationships. The table shows the relationship between the indicator variable and ACH.
Timing is another matter. Except for traffic cycles, a major source of outdoor air pollution, outdoor air pollution episodes tend to occur over days; the indoor, low-flow processes tend to operate on hourly time scales. Even though indoor-outdoor relationships may differ widely within a community, “bad (outdoor) air” days would likely be experienced throughout.
Lamp Post Syndrome
Long-term health effects of air pollution have traditionally been evaluated through population-based epidemiology studies that compare health and outdoor air quality by location. Such studies are thus about places but not necessarily their inhabitants. Personal exposures would require long-term data from thousands of residences in which indoor and outdoor air quality were continually monitored along with occupant health and are thus costly and intrusive. EPA studies outdoor air because it’s much easier to do so (“the light is better under the lamp post”), not because it’s relevant to public health.
Homeowners need to know that their environments are safe. Building codes have responded by requiring interior smoke alarms and carbon monoxide (CO) monitors. The concept of monitoring residential air is well-established and inexpensive instruments have been developed and widely deployed for those two regulated outdoor pollutants [3]. Conversion of these alarm systems to continuous reading instruments could provide indoor exposure data for use in epidemiology studies.
It's time to put up or shut up!
For years, the EPA and World Health Organization (WHO) have been lecturing us about the putative economic costs of “bad” air quality, typically in the billions or trillions of dollars. It’s now time for agencies to provide real, not estimated or modeled, indoor air quality data that will extend our science base.
[1] Lipfert FW. An assessment of air pollution exposure information for health studies. Atmosphere 2015, 6, 1736-1752.
[2] Yamamoto et al. Residential air exchange rates in three major US metropolitan areas: results from the Relationship Among Indoor, Outdoor, and Personal Air Study 1999-2001. Indoor Air. 20(1) 2010 85-90.
[3] “Smoke” is an important constituent of PM2.5 and perhaps the most important one, based on the lethal episodes of the past century. Ozone and SO2 react with indoor surfaces and thus do not pose indoor air quality issues.