A group at the University of Houston has discovered a vaccine that blunts the effect of fentanyl in mice, making it a potential tool for combating the deadly fentanyl overdose epidemic that continues to plague the US. Its development is only at a very early stage and may or may not ultimately work in humans, but if it does, how will it be used? It's not so simple.
First, a little science.
Simple organic chemicals or drugs rarely (1) elicit an immune response; these molecules are too small to be recognized by the immune system, which is "on guard" for much larger invaders like viruses and bacteria. But there is a method that can "trick" immune cells into forming antibodies recognizing small molecules like drugs. This is a so-called hapten approach. Haptens are small molecules/drugs (in this case, fentanyl) that can be attached to proteins via a covalent bond to form a stable drug-protein conjugate.
Injecting conjugates, which are large enough to be recognized by receptors on immune cells, can then induce the formation of antibodies. But these antibodies not only recognize the protein-fentanyl conjugate; they also recognize fentanyl itself, which provides a way for antibodies to clear the drug from the blood via the kidneys. Here's a simple diagram of how it works (Figure 1).
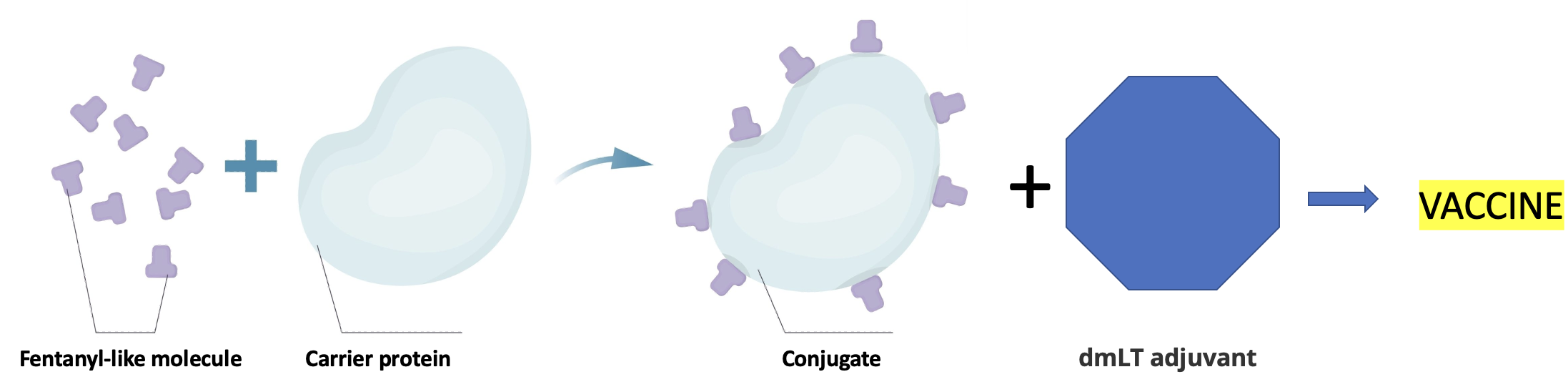
Figure 1. Original image credit: Standard license from Shutterstock. In Figure 1, the hapten is a fentanyl-like molecule (2) attached to a carrier protein. The Houston group used a standard, FDA-approved protein called CRM-197 to synthesize a stable conjugate with fentanyl. While conjugates themselves elicit an immunological response, this can be enhanced (standard vaccine science) by adding an adjuvant, in this case, an FDA-approved adjuvant called dmLT. The mixture of the conjugate plus the adjuvant made up the vaccine, which formed functional antibodies when injected into mice. (You may or may not want to know how it was determined if the vaccine worked. If so, you can read about it here. It involves rather gruesome animal experiments.)
Specificity - The fentanyl vaccine did not neutralize opium-based analgesics (or the other way around)
The researchers also made conjugates of naturally-occurring opiates, semi-synthetic analogs and methadone as controls. These opiate conjugates, plus the adjuvant, generated antibodies in much the same way, but none of them blocked the action of fentanyl. This is exactly what would be expected since the hapten-carrier complex presented a fentanyl-like molecule, not an opiate-like molecule, to the immune system. Since the chemical structures of opiates and fentanyl are entirely different, it would be very strange if the immune system recognized morphine-based conjugates. But the vaccine did neutralize sufentanil, which would be expected based on its structural resemblance to fentanyl (Figure 2).
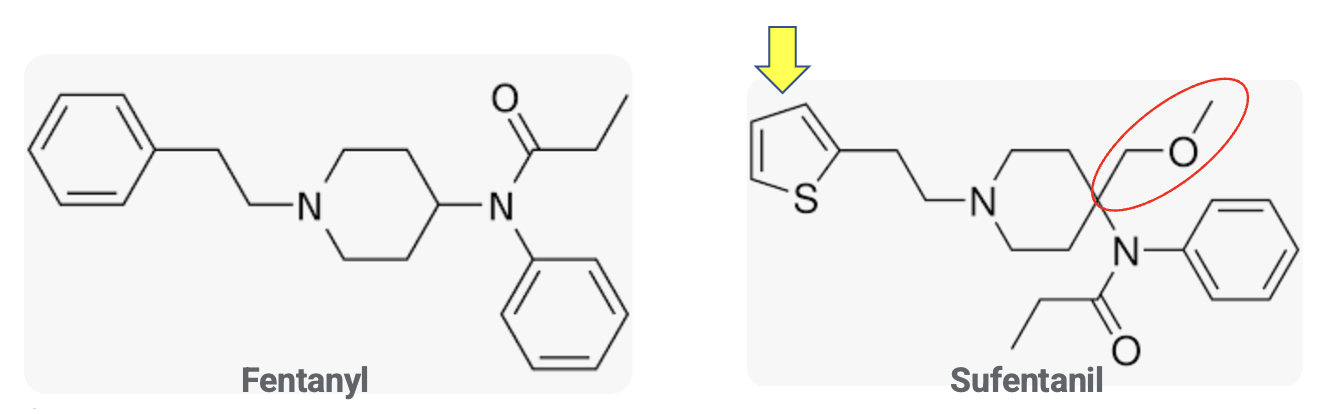
Figure 2. The chemical structures of fentanyl and sufentanil. The yellow arrow indicates the thiophene group that replaces a phenyl group in fentanyl. The red oval (methoxymethyl group) represents the only substantive structural difference between the two drugs.
To someone who is not trained in organic chemistry, fentanyl and sufentanil may look somewhat different, but in reality, they are nearly identical. The only significant difference between the two drugs is the methoxymethyl group (red oval). Although the benzene and thiophene (yellow arrow) rings may look different, they are isosteres – different molecules with similar chemical properties. So it is not at all surprising that antibodies generated by a fentanyl vaccine would recognize sufentanil but not morphine or any of the other opioids. This specificity is clearly shown in Figure 3.
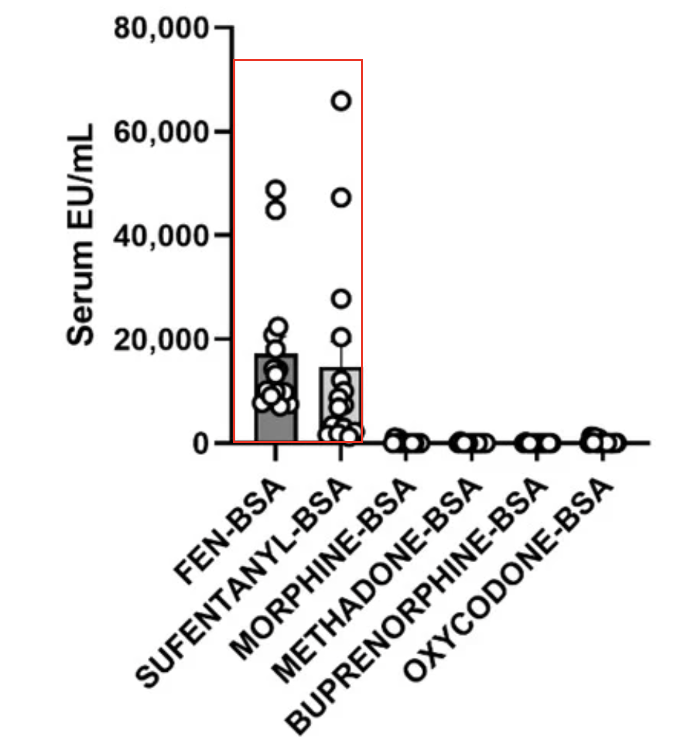
Figure 3. Anti-fentanyl antibody specificity in samples from vaccinated rats. Source: Pharmaceutics, 2022.
How would such a vaccine be used?
If the fentanyl vaccine is found to be safe and effective in humans, this raises some intriguing questions, the most obvious of which is how would it be used.
- General public
No way. While vaccines for infectious diseases, such as flu, measles, and pneumonia, are available (and should be used) as public health measures, the same cannot be said for a fentanyl vaccine. People who don't use street drugs are unlikely to seek protection from them. To make matters worse, such a vaccine would nullify the medical use of fentanyl, either for severe pain control or anesthesia. The NIH estimates that 3 million people in the US have (or have had) opioid use disorder. Of this number, 500,000 people are estimated to be addicted to heroin. The number of people who a fentanyl vaccine might protect will likely lie somewhere in between these two numbers, representing well less than 1% of the US population. In no way does it make sense to vaccinate 99+% of the country to protect those at risk.
- Addicts and recovering addicts
It is unlikely that hard-core heroin addicts, many of whom are homeless and have medical and psychiatric diseases, will seek such a vaccine; they are more concerned with getting their next fix than taking measures to protect their health.
But for people addicted to opioids and trying to quit, the vaccine could provide a safety net in case a relapse sends people back to street dealers. In a way, this is analogous to using methadone to mitigate the harm from more dangerous drugs. People in this group would benefit greatly from a fentanyl vaccine.
- "Casual" drug users
There are far too many news stories of partying teenagers buying what they think is oxycodone and ending up overdosing from fentanyl in what turned out to be counterfeit pills. A fentanyl vaccine could be beneficial here, although the idea of seeking protection from one illicit drug so that others can be more "safely" used is a bit odd.
But even this group would not necessarily want to be vaccinated. A 2022 NBC report discusses how fentanyl, once feared, has become a sought-after drug, especially for smoking. It goes without saying that fentanyl smokers are unlikely to be eager to take a vaccine that will counteract the effects of the drug.
Bottom line
While a vaccine to protect people from drugs may be a foreign concept to most of us, the science behind this research makes perfect sense. Whether the results in mice can be duplicated in humans and, if so, how such a therapy would be used remain unknown.
NOTES:
(1) One notable exception is urushiol, the active component in poison ivy—sort of. Urushiol itself does not cause the reaction; it is the oxidation product that covalently binds to skin proteins and causes the immune response.
(2) Fentanyl itself has no "handle" to attach a linker to the protein. Instead, a derivative with a carboxylic acid "handle" was prepared according to a literature method. The carboxylic acid can be reacted with amino groups on the protein.





