As a physician, I have long advocated that healthcare workers, in particular, be vaccinated to reduce the risk of transmission to our patients – it is part of Do No Harm. A new study reported in JAMA Network Open puts some numbers to my belief. The researchers used a variety of data sources, linking them to the National Healthcare Safety Network, which has weekly vaccination, cases, and deaths attributable to COVID-19, for nursing home staff and occupants.
They confined their dataset to two periods: relatively early, when the vaccine became more widely available (May-December 2021) and when Omicron made those vaccines less effective (December 2021-January 2022). The data included 15,042 nursing homes, with a mean staff vaccination rate of 66% and a mean quality rating by CMS (Nursing Home Compare) of 3.26 – slightly better than average. The counties surrounding these facilities had a weekly prevalence of 0.25 cases/per 1000 population.
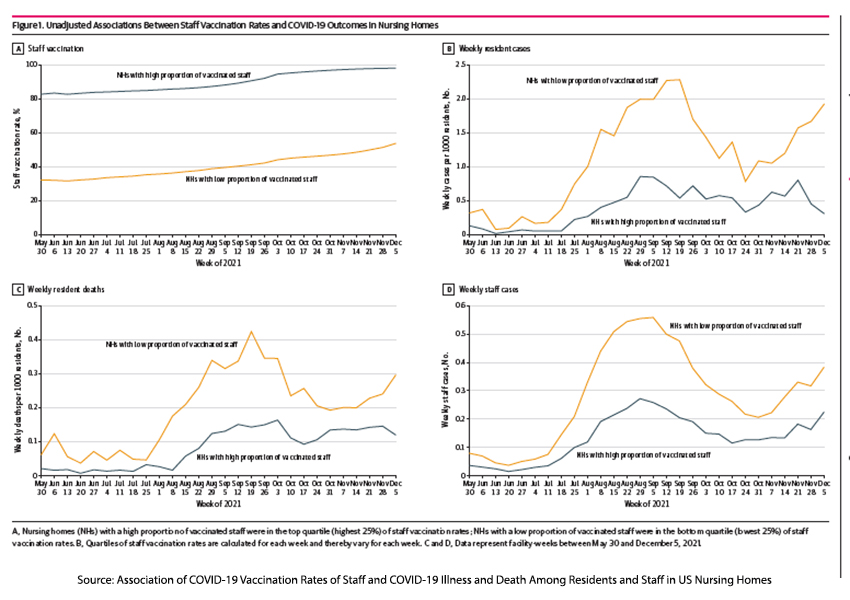
- Vaccination rates among the staff showed significant variation; the lowest percentile vaccination rate at the beginning of vaccination was 32%, the highest percentile 82%. Over time, both of these vaccination rates improved, but the 50 percentage points gap between lowest and highest was reduced only slightly to 44%
- Facilities with the highest vaccination rate among staff had “lower levels of weekly COVID-19 cases and deaths among residents and a lower level of weekly COVID-19 cases among staff.”
- This association did not continue during the Omicron wave.
- An increasing prevalence of cases in the community resulted in increasing cases within nursing homes.
- Increasing hours spent with nursing home staff also reduced resident cases and deaths. [1]
The finding that increasing staff hours spent with nursing home residents resulted in fewer deaths is a bit puzzling. You would think that more prolonged periods of exposure would result in greater transmission; perhaps just as there may be a threshold of exposure, there may be an upper limit where transmission does not increase. And we do not know which healthcare workers increased their care hours. That makes a difference because when we consider healthcare workers’ roles, nurse's aides trail behind nurses and physicians in being vaccinated. On the other hand, perhaps those extra hours provided additional care to residents who were not as frail and could survive a COVID-19 infection.
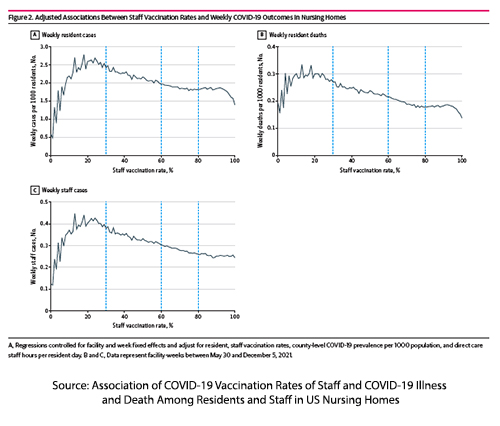 Another interesting finding in the study was an apparent dose-response to vaccination that might reflect the tipping point towards a nursing facility’s “herd immunity." It appears that at roughly 30% vaccination for nursing home staff, weekly cases among both staff and residents, as well as resident deaths began to decline.
Another interesting finding in the study was an apparent dose-response to vaccination that might reflect the tipping point towards a nursing facility’s “herd immunity." It appears that at roughly 30% vaccination for nursing home staff, weekly cases among both staff and residents, as well as resident deaths began to decline.
Of course, no study like this would fail to extrapolate their findings to larger time frames and numbers. Over one year, a 10% increase in staff vaccination would reduce cases by 10% per thousand residents and deaths by 15%. These are not trivial numbers; flipping the script, no one would undertake an operation with a 15% mortality.
The fact that the initial vaccination was ineffective in reducing the transmission of Omicron suggests that it requires effective vaccines to reduce cases and severity and protect nursing home residents – and the initial vaccine wasn’t. It supports the need for healthcare workers to be boosted with newer vaccine iterations that have greater efficacy against newer variants.
For me, the bottom line is that this study is evidence that vaccination of healthcare workers reduces harm to those under our care. We have an ethical obligation to be vaccinated; it is not the ethical principle of non-Maleficence; it is "do no harm" that is important. The principle of beneficence to do good is ascendant in these circumstances.
[1] Most time spent with residents is with nurse's aides, 60% of the 4 hours of “nursing contact.” Registered nurses spend 18% of the time and licensed practical nurses the remainder.
Source: Association of COVID-19 Vaccination Rates of Staff and COVID-19 Illness and Death Among Residents and Staff in US Nursing Homes JAMA Network Open DOI:10.1001/jamanetworkopen.2022.49002