I’ve written in the past about COVID among healthcare workers. Beyond the fear-mongering headlines of a 7-fold higher rate of COVID infections among healthcare personnel, we find that most of COVID’s carnage was visited upon nurses and their aides. Physicians’ risk was slightly higher than that of a medical technician and somewhat lower than the staff providing environmental services.
A research letter published in JAMA Internal Medicine looks at the excess mortality of physicians from March 2020 to December 2021 from AMA files of physicians and deaths during that interval. With a monthly average of 750,000+ physicians, the researchers calculated an excess of roughly 622 deaths from a total of 4511.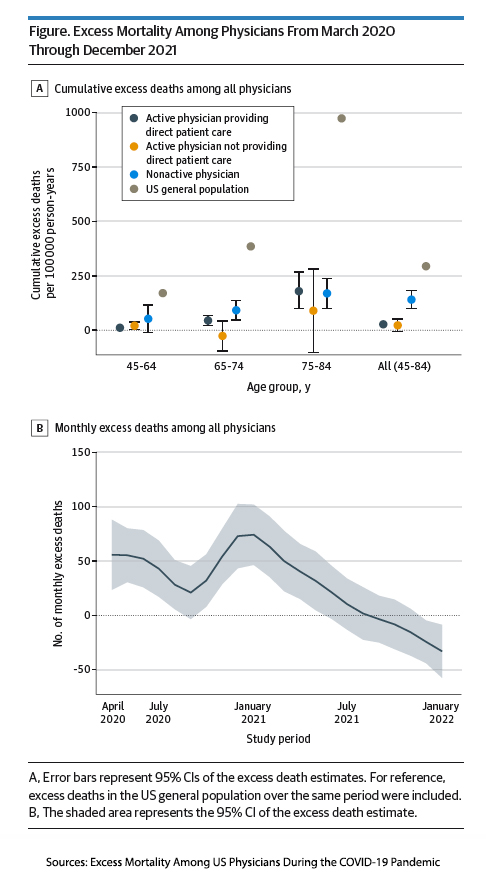
- The picture tells the story. Physicians in all age groups fared better than the general public of the same age.
- Active physicians providing or not providing direct patient care fared equally as well.
- Nonactive physicians, presumably those retired by age or disability, fared the worst.
Why might this be the case, especially for those physicians on the front line delivering face-to-face patient care?
As the authors suggest, I would argue that it was their work environment, which involved wearing protective clothing and masks to lessen the transmission of the virus along with, I am sure, more scrupulous handwashing than physicians are typically known for. And here is a fun fact from the second graph of monthly excess deaths. There were no excess deaths after April of 2021, “coinciding with the widespread availability of COVID-19 vaccines.”
There are other sequelae of COVID among healthcare workers. The common narrative has been that many physicians have retired due to COVID. A closer look suggests that an already aging workforce accelerated their retirement more than simply deciding to quit – for patients, that may be a difference without a distinction. Physicians are not immune to burnout, although calling it post-traumatic stress might be a better term. 40% of practices say physicians have left because of PTSD or early retirement.
Physicians leaving practice exacerbate a physician shortage, especially in primary care. That will result in more urgent-care, doc-in-a-box facilities where physicians can have a better work-life balance, but patients will lose continuity of care. It will result in a shift to nurse practitioners and physician assistants (or, as they often choose, associates) being our primary care providers. It will create an opportunity for foreign-born and trained physicians to work here, further draining their home countries' healthcare resources.
Like a rock dropping into a pond, the impact of COVID on healthcare personnel continues in ever-widening circles.
Sources: Excess Mortality Among US Physicians During the COVID-19 Pandemic JAMA Internal Medicine DOI: 10.1001/jamainternmed.2022.6308




