The strongest evidence that high pollution levels can accelerate mortality came from the Great London Fog of 1952. [1] This association was confirmed by experimental evidence:
- Indoor air was so severely polluted that cinema projections could not reach screens.
- The mortality rate was so high that 90% of the dead were fog victims.
- Autopsies showed black smoke particles in their lungs.
- Those autopsies also showed evidence of pre-existing cardiopulmonary diseases.
This event spawned thousands of studies of daily variability in specific causes of sickness and death and various air pollutants.[2] Most involved time-series analysis with statistical control of season and daily weather effects. In 2020 I published a review of air pollution-mortality studies that contrasted estimates based on daily exposures with those based on annual data [3]. Recent publications suggest that even finer time scales should be considered. Here we address questions of exposure timing.
Short-term (hourly) exposures.
Controlled experiments provide more robust evidence than statistical inference, but there are serious practical limitations. Healthy individuals can be subjected to exposures of limited duration to pollutants created in the laboratory for reversible health endpoints. Hourly exposures are problematic for ambient PM2.5 because that period is too brief for an adequate sample of particles.
- Diesel smoke. Forty-five nonsmoking subjects aged 18-49 were exposed to 200 μg/m3 diesel smoke particulates for 2 hours while changes in blood pressure were noted. Systolic pressure increased by 4.4 mmHg 30-60 minutes after exposure and remained high for ~20 hr. There were no effects on diastolic pressure or heart rate. This level of exposure would be equivalent to a daily mean increment of about 17 μg/m3; the current mean urban levels are generally < 1 μg/m3.
- Indoor air cleaners. High-efficiency particulate air filters were installed in the rooms of 24 healthy residents of a senior care center for two days. Air filtration was associated with significantly decreased biomarkers of inflammation and coagulation but not with oxidative stress or lung function.
- Fireworks. Airborne particulate matter was measured during New Year celebrations in the Netherlands and reached 300 to 600 μg/m3 over an hour. No consistent associations were found with subsequent daily mortality in the general population.
- Ambient air quality. Onsets of acute coronary syndrome in 1.3 million Chinese were compared with hourly outdoor concentrations of PM2.5, coarse PM, NO2, SO2, CO, and O3. Associations were strongest for the elderly in winter and the concurrent hour of exposure, declining after that. Associations were weak for NO2, PM2.5, and O3,
- Concentrated ambient particles. EPA tested groups of healthy human volunteers with increased concentrations 6-10 fold over several hours. Responses included mild inflammation, varied within groups, and were more substantial with elderly subjects. No deaths or hospitalizations were reported.
These studies indicate that acute air pollution exposures can affect health, depending on the recipient, types of exposures, and outcome measure, but do not reflect life-threatening levels.
Multi-day exposures.
Analyses of daily health outcomes and coincident air quality began with the 1952 London fog episode and continue to this day. Early studies struggled with confounding of pollution events by season, weather, days of the week, and holidays. Nevertheless, this epidemiology model resembles a population-based experiment in which a dose is administered and then relieved, with time-series analysis determining the extent to which outcomes follow exposures.
The missing link here is the identification of victims. Daily urban death rates are in double digits, of which only a few percent may be associated with bad air quality. The usual method of time-series analysis is to limit the analysis to those over age 65 and, more recently, additional stratification by frailty status.
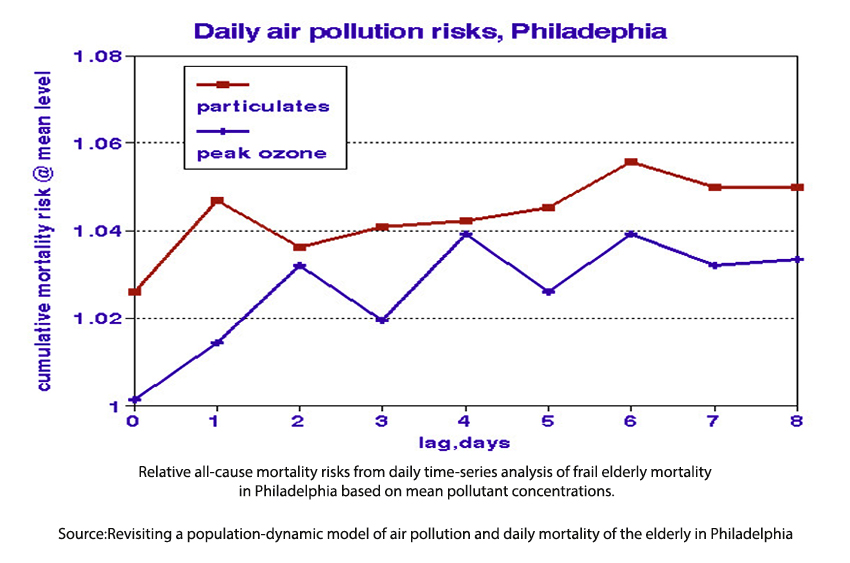
These studies find statistically significant relationships with ambient air quality (see graph) limited to frail members of the population such that their lives were cut short by only a few days. The Philadelphia graph shows that additional frail people died on the days following exposure, summing to about 5%.
Perhaps the most important finding of these studies is the common-sense notion that frailty and exposure are partners in premature mortality. In a diverse population, there will likely always be an individual frail enough to succumb to peaks in current ambient air quality levels, which could explain the persistent inability of air pollution epidemiology to find “thresholds” of no effect. Given bad enough air quality (as in 1950’s London), frailty may no longer be an issue, and ostensibly healthy people may be struck down.
Annual and historical exposures.
Most estimates of the chronic effects of air pollution have been based on long-term differences among cities, the so-called cross-sectional studies. They usually contrast exposures and responses without considering cumulative effects or latency of disease development. Nevertheless, such associations have consistently been interpreted as showing that air pollution causes disease. In contrast, the correct conclusion may be that unhealthy locations are more polluted than healthy ones.
Experimental confirmation of a cross-sectional effect would require transferring a population to a less (or more) polluted area for several years and back again, noting any changes in health status after accounting for differences in age, smoking, income, etc. Such an experiment would clearly be impractical and probably unethical. However, controlled experiments on monkeys and guinea pigs inhaling high levels of SO2 and fly ash for up to 78 weeks found no related adverse effects. Cumulative responses or time-weighted averages are the appropriate long-term exposure metrics, e.g., pack-years in smoking studies or working-level years in radon or occupational studies.
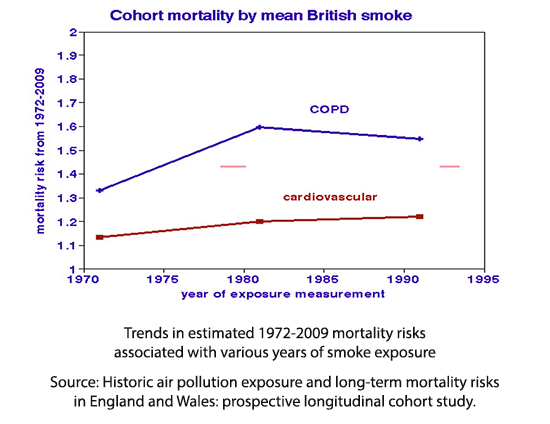 Cross-sectional studies of differences among cities typically find air pollution relationships around 10% ascribed to long-term effects such as the development of a new disease like arteriosclerosis. However, causing a truly long-term effect would require decades of prior exposure. This graph shows how ~40 y mortality relates to cohort exposures during various periods; differences are modest and suggest that recent exposures may be more critical. Only three truly long-term cross-sectional studies considered associations of historical air pollution exposures on mortality rates during successive periods. They reported no evidence of cumulative or delayed effects.
Cross-sectional studies of differences among cities typically find air pollution relationships around 10% ascribed to long-term effects such as the development of a new disease like arteriosclerosis. However, causing a truly long-term effect would require decades of prior exposure. This graph shows how ~40 y mortality relates to cohort exposures during various periods; differences are modest and suggest that recent exposures may be more critical. Only three truly long-term cross-sectional studies considered associations of historical air pollution exposures on mortality rates during successive periods. They reported no evidence of cumulative or delayed effects.
Summary
The studies reviewed here point to “here and now” for the adverse effects of air pollution.
The role of short-term as an essential part of long-term effects has not been recognized in risk analysis. What happens over the long-term ipso facto includes what happened in the short term. Any actual long-term effect should be characterized by the difference between long- and short-term estimates, taking into account the uncertainties in each. Since daily effects have often been underestimated by failing to include sufficient lag periods, and long-term effects may have been overestimated by failing to control for differences in historical exposures, or indoor air quality, such differences may not be statistically significant. The long-term impact of PM2.5 have not been supported by direct experiments; plausible physiological mechanisms are thus lacking. Chronic diseases require decades to develop, but the few mortality studies that considered exposures in prior decades reported that recent exposures were the most important, suggesting that acute effects dominate.
“We did not find that exposures in early life has (sic) a multiplicative effect on mortality risk associated with more recent PM10 exposure.”
Suffice it to say that air pollution can affect health under specified conditions of source and receptor, but confirmation of long-term causality remains elusive.
[1] Lipfert FW, Air Pollution and Community Health, Wiley, New York (1994).
[2] The NIH PubMed database showed 1300 time-series publications, 199 of which controlled for day-of-week effects, 32 mentioned indoor air, 9 mentioned frailty, and none mentioned autopsy.
[3] Lipfert FW. Air Pollution and Mortality: Timing Is Everything. Atmosphere 2020, 11, 1274



