The Wall Street Journal published a news article on January 5, “Why It Feels Like Everyone You Know Is Getting COVID-19,” which contained several worrisome observations. It cited “a seven-day average of more than 26,000 people hospitalized with COVID in late December, about double the number two months earlier,” noting that although the numbers of hospitalizations and deaths are far lower than during the previous two winters, “it remains a disruptive and rapidly spreading illness.”
Those were understatements. Within hours after the article appeared, the CDC released updated December numbers that were significantly worse. During the week from Dec 24-Dec 30, COVID hospitalizations were up 20.4% week-over-week, with almost 35,000 hospitalizations that week. COVID deaths were up 12.5% from the previous week. And the curves were clearly trending upward, with the full impacts of holiday super-spreader events not yet evident.
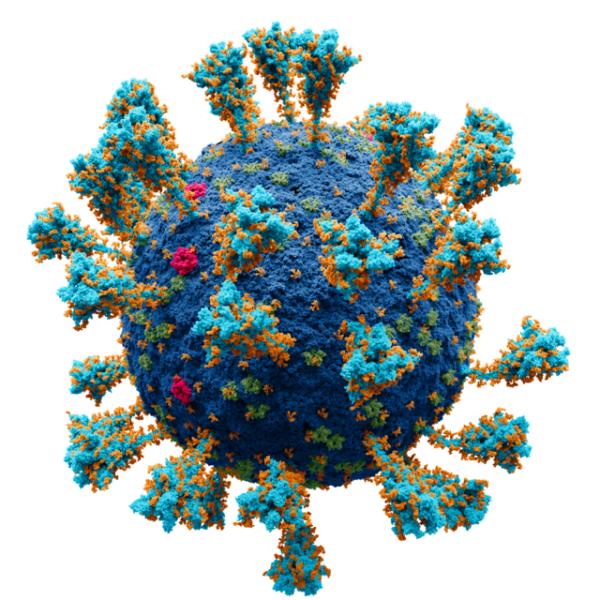
Another worrisome trend is the concentration of SARS-CoV-2, the virus that causes COVID, in wastewater, which is an early predictor of future infections:
Leaving aside the predictive value of wastewater analysis, it can also be used to estimate the number of infections in real-time. According to infectious disease modeler J.P. Weiland, the U.S. was experiencing more than 1.5 million cases of COVID daily (and trending upwards) as of December 31:
Data from Biobot and CDC
None of this is surprising for several reasons. First, we are in the throes of a worldwide expansion of a new, hyper-mutated, immune-evasive variant of Omicron called JN.1, which now accounts for about two-thirds of U.S. cases (and causes symptoms similar to those caused by previous COVID variants -- cough, fever, body aches, and fatigue.) Fortunately, there is some cross-reactivity for neutralizing antibodies between JN.1 and XBB.1.5, the virus whose spike protein is in the most recent COVID booster, which is why the most recently-offered booster (introduced last September) induces some immune response that might otherwise not have occurred. But, as Scripps Research’s Dr. Eric Topol says: “That’s luck, folks. It may not happen again with the next ‘updated’ booster in 2024 or 2025.”
Second, although the numbers are not (yet) as bad as they were in previous winters, the fact remains that with appropriate precautions to “flatten the curve” of infections, many COVID cases, hospitalizations, and deaths would be preventable. But only 19% of eligible Americans have gotten the most recent COVID vaccine booster, and masking is almost non-existent even in high-risk situations such as airports, airplanes, trains, theaters, and other places where people congregate indoors in large numbers.
Another point regarding the prevention of bad outcomes from COVID infection is the low percentage of physicians prescribing the drug Paxlovid for people who become infected. Paxlovid prevents the COVID virus from replicating and stunningly reduces the risk of severe infection, hospitalization, or death. It may also lower the probability of an infection leading to the persistence of signs and symptoms after the acute infection has passed – that is, “long COVID.” The results of a large study published in March 2023 found that in the 282,000 people in the study who were eligible for Paxlovid, the drug reduced the incidence of long COVID by 26%.
However, physicians have been underprescribing the drug, both because they don’t know much about it (or about long COVID) and because it can interact negatively with numerous other drugs. (These interactions can usually be successfully managed, such as by briefly stopping or changing the dose of the other drug.)
Long COVID is not only potentially debilitating and life-threatening to individual sufferers but also constitutes a significant challenge to our healthcare system. As Dr. Topol wrote on January 5:
There isn’t adequate acknowledgment of the risk of Long COVID — or the protection [afforded by] vaccination. When you think of up to 2 million Americans getting infected in a day, even if only 1% go on to suffer from chronic COVID, which can be profoundly debilitating, that’s 20,000 eventual new long haulers added to the millions here already affected. In one day. The current wave has gone on for weeks and estimates are that 4-5% of Americans have Covid now and up to 1 in 3 will have been infected during the wave cumulatively.
Finally, officials at the top of the nation's public health food chain, including the U.S. Surgeon General, HHS Secretary, and the directors of the CDC and FDA, have not been aggressively urging Americans to take appropriate precautions. Their negligence is allowing the pandemic to accelerate.
A public health bonus of more responsible behavior – namely, vaccination and masking in high-risk situations – would be suppression of flu and respiratory syncytial virus, or RSV, the other two serious respiratory infections currently circulating at high levels. Only about 45% of adults have been vaccinated against the flu this season, and at least 10 million people in the U.S. have gotten the flu so far, resulting in about 110,000 hospitalizations and 6,500 deaths. RSV vaccination rates have been even more dismal, with only about 18% of adults over 60 receiving an RSV shot.
Mask mandates for staff and patients in healthcare facilities are finally beginning to be reinstated across several U.S. states, but these efforts are likely too little, too late for the nation as a whole.
As my fellow Philadelphian Benjamin Franklin counseled in 1736, “An ounce of prevention is worth a pound of cure.”



