
Cholesterol levels in the blood are widely acknowledged indicators of heart disease risk. According to the National Institutes of Health (NIH), the ideal level of LDL or "bad" cholesterol is anything less than 100 mg per dl (100 ccs of blood). But for so-called "good" cholesterol, the HDL, anything above 60 mg/dl is considered protective against heart disease. That's because HDL facilitates removing cholesterol from cells lining the arteries and transporting it back to the liver, thus reducing the risk of blocked arteries.
Some research (for example here) questions whether that prescription really holds, though, and suggests that you can have too much of this particular "good thing." And now a recent study published in the European Heart Journal depicts what seem to be the optimal levels of HDL for men and women.
Danish researchers, led by Dr. Børge G. Nordestgaard from the University of Copenhagen, used data from two large prospective studies to analyze possible links between high levels of HDL cholesterol and risk of death from any cause. In particular, they were interested in learning if people with extremely high levels of HDL were at a greater risk of dying than people with lower levels. The data they used was derived from the Copenhagen City Heart Study and the Copenhagen General Population Study, with median follow-ups of 6 years. They included over 52,000 men and over 64,000 women.
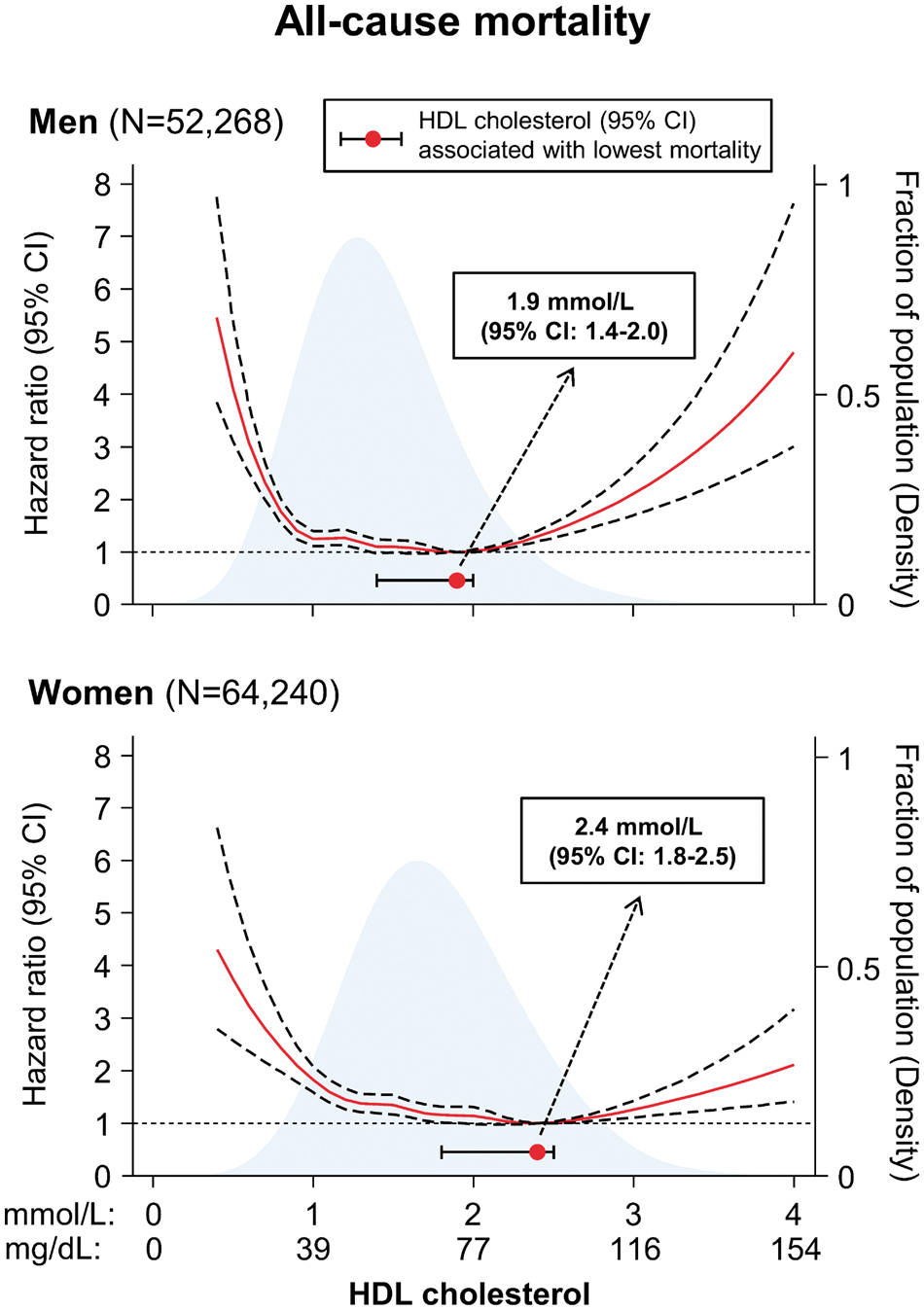
They also determined the risk of death for men and women separately according to levels of HDL — and found that in both genders these resulted in U-shaped curves, indicating that both the lowest and highest levels of HDL were associated with increased mortality. See chart below.
During those studies, about 5600 men and 5000 women died — mortality rates of 17 and 12 per 1000 person-years respectively.
And the lowest risk of death was associated with HDL levels of about 58 and 77 mg/dl for men and women respectively.
But compared to those with these “optimum” levels of HDL, those with extremely high HDL levels had increased cardiovascular mortality risks — hazard ratios of 2.5 in men and 2.9 for women.
Of course, these are observational studies, so one can’t interpret these data to mean that extremely high HDL levels cause the increased risk of death. Further, these data were derived from a Caucasian population, and may not apply to other groups.
In their discussion, the authors state:
Our results indicate that the common belief that, the higher the concentration of HDL cholesterol the better, does not hold for extreme high concentrations, as the relationship between HDL cholesterol and all-cause mortality was not linear over the entire range of HDL concentrations. Secondly, if the association between extreme high HDL cholesterol and high risk of death is causal, these findings would add to the uncertainty regarding elevating HDL cholesterol pharmacologically to extreme high concentrations.
Thus, as with vitamins and chocolate, it seems that the idea that “a little is good, but a lot might be harmful” could apply to HDL cholesterol too.
Whether the association between extreme high HDL cholesterol and increased mortality is causal is an important unresolved question concerning the findings in this study.



