Mutants are everywhere. And no, I’m not talking about the creatures you find in video games, comic books, or Saturday morning cartoons. We’re the real mutants—you, me, and everyone you know. It’s a fundamental part of being alive.
Though the term has a pejorative connotation, mutations are just changes in DNA. They may sound scary, but they’re a common by-product of cell division. Each of the trillions of cells in your body contains billions of DNA bases (“letters”) that comprise your genetic code. The DNA replication machinery is extraordinarily accurate (1), but roughly two trillion cell divisions occur every day, so there are tons of opportunities for it to make mistakes. The handful of errors that do slip through the cracks will get passed along every time the mistake-bearing cell and its progeny divide. Most of these mutations don’t change anything—and some are even beneficial—so it’s not something to lose sleep over. Just don’t expect to turn into a crime-fighting, pizza-loving turtle anytime soon.
If you’ve read my previous two articles, you may see where this thread is going. As we discussed last week, cancers are caused by DNA mutations that cut the brake lines and/or floor the gas pedal on cell proliferation. The nature of these mutations—among other factors—can alter cellular behavior so dramatically that the term “cancer” actually refers to many different diseases. Therefore, the traditional tissue-of-origin-based classifications (breast cancer, lung cancer, etc.) may not be as informative as the clues found in cancer cells’ DNA.
But it’s even more complicated than that. Because cancers are such good genetic shapeshifters, a single patient can house distinct groups of cancer cells that behave differently from one another. One potential cause is metastasis, the process by which cancer invades other areas of the body (2). But cancer doesn’t need to spread for multiple cancer cell types to form—they often exist within the same tumor.
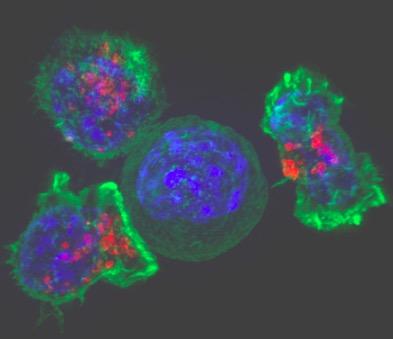
Many cancers manifest as solid tumors, (3) which are lumps of abnormal cells whose growth and behavior are not regulated by neighboring tissues. A tumor may seem like a single entity on the macroscopic level, but increasingly sophisticated research techniques have revealed that tumors are actually highly heterogeneous; they contain multitudes, and that’s bad news for patients.
A common driver of tumor heterogeneity is a phenomenon known as genome instability. Some of the cancerous mutations that trigger uncontrolled cell growth also increase the likelihood that additional mutations will arise. Because many (if not all) of the cells in an “unstable” tumor harbor this increased propensity for genetic change, different sets of mutations will accrue and propagate independently as the cancer grows. The result is a collage of cell types that exhibit an increasingly wide set of behaviors.
Instability-promoting mutations are often found in the aforementioned DNA repair mechanisms that keep the error rate in check during DNA replication and cell division. Two of the most well-known genes involved in this process are BRCA1 and BRCA2. A harmful mutation in either gene is associated with a dramatically increased risk for breast and ovarian cancer; on average, 50-85% of women with a faulty BRCA1 or BRCA2 gene will develop breast cancer by age 70.
High variability can be problematic from a treatment perspective. If you give a cancer cell more rolls of the mutagenic dice, then it’s more prone to spontaneously acquire a mutation that makes it more aggressive and/or resistant to therapy. As a result, it’s likely that not all of the cells in a given tumor will respond to the same drugs. Even worse, the ones that survive, grow back, and cause disease relapse will probably be resistant to everything you’ve already thrown at them. Thankfully, genome instability presents its own set of vulnerabilities, but oncologists are still figuring out how to exploit these new weaknesses as effectively as possible.
Returning to the theme of this series, tumor heterogeneity presents some damning evidence against a universal cure for cancer. It seems unlikely, to say the least, that a single drug will be able to circumvent a core aspect of cancer biology that essentially generates different diseases within the same patient. There are plenty of reasons to be optimistic about the future of cancer treatment, but that optimism should be guided by a realistic sense of what’s scientifically possible.
NOTES:
[1] The error rate is roughly 1 in 100,000 bases. This seems really impressive, but the mathematically adept will realize that this adds up to ~120,000 errors across the 6 billion base pairs in the human genome. Thankfully, there are various proofreading and error repair mechanisms that lower the error rate dramatically.
[2] This is a complex, fascinating, and important topic that deserves its own article—stay tuned!
[3] Leukemias and other blood cancers are notable exceptions.


