In the world of infectious diseases, it is always better to prevent an infection than to treat it. Almost without exception, this means vaccination is the way to go (1). But it's not so easy. Far from it. Here's a look at how science has performed so far in response to the Wuhan coronavirus. And why even the best efforts might not make a difference.
1. The Speed. Wow.
The genome of the virus was determined with lightning speed and published immediately (January 11th) by Professor Yong-Zhen Zhang of the Shanghai Public Health Clinical Center & School of Public Health at Fudan University in Shanghai. But the credit does not belong solely to Zhang. Far from it. In this case, we saw the power of collaborative science (2) among different groups in multiple countries.
The timeline of the period between the discovery of 2019-nCoV/Wuhan virus and where we stand now sounds like it comes from a science fiction script, but it's real:
- December 2019 – An outbreak of viral pneumonia hits Wuhan. No one has any idea what was the causative pathogen.
- January 9, 2020 – Chinese scientists and the WHO announced the discovery of 2019-nCoV (aka Wuhan Virus) and confirmed that it was responsible for the cases of pneumonia.
- January 11 – China releases the genomic sequence. The genome was determined from samples isolated from the first patients. It is freely available (3).
- January 24 – Scientists at The Pasteur Institute in Paris begin sequencing the viral genome from samples taken from three French patients. They begin on Friday and have the sequence solved by Monday (!).
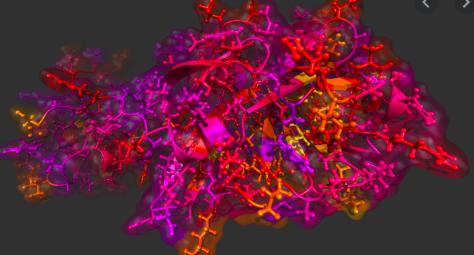
- January 30 – The Pasteur Institute scientists release the viral genome, which confirms that it's the same virus that infected Chinese patients. Here's what the genome looks like.
Credit: INSTITUT PASTEUR / CNR OF RESPIRATORY INFECTION VIRUSES.
- January 29 – An Australian announced that it was able to grow the virus in cultured cells. This is enormously important for the development of diagnostic tests, vaccines, and antiviral drugs. I'll get to that in a moment.
2. Now Comes the Hard Part
There has been talk about having a vaccine against the coronavirus in months. I hope I'm wrong, but this sounds delusional. The Coalition for Epidemic Preparedness Innovations (CEPI) in Norway is funding Moderna Therapeutics and Inovio Pharmaceuticals, two biotechs. CEPI says they hope to have a vaccine candidate ready for human testing in 16 weeks (!). But even if they succeed there is a big difference in having a Phase I candidate and an approved, working vaccine.
The previous record for the fastest vaccine development goes to Inovio. But the company also gets an award for the fastest dose of hard luck. In response to the Zika threat in 2015, the company had an experimental vaccine ready to be tested in humans in seven months. Except it didn't matter. Zika largely dissipated and the vaccine was left on the shelf. It made no sense to run clinical expensive trials for an infection that "went away." Just one of the many things that can go wrong in the world of drug and vaccine development. You can succeed and still fail.
3. All this can go wrong too...
The ability to grow viruses in vitro (outside the body) is critical to vaccine and drug discovery. If Compound X stops influenza from growing in a dish of cultured cells it has a chance to do so in animals and humans. Here's how it works: biologists seed a monolayer of cultured host cells with a virus and measure how well the virus grows with and without X being present.
Ironically, norovirus (stomach virus), the evil little SOB, which is one of the most contagious pathogens in the world, absolutely refused to grow in cultured cells, and this is almost surely a reason why we have neither a vaccine or antiviral drug for the infection. It took 50 years to overcome this problem. Hepatitis C, which infects the livers of 3% of the people in the world, would not grow in liver cells (seriously?). A stripped-down, artificial version of the virus called the HCV replicon was synthesized and this discovery led to drugs that cured the infection. But the discovery of the HCV replicon took about 10 years.
Human papillomavirus (HPV), the most common STD in the US is highly contagious, but there still isn't a good way to grow the virus outside the body. On the other hand, some viruses grow like gangbusters in cultures of host cells. So do influenza, measles, herpes, and varicella-zoster (chickenpox/shingles).
And there are some pathogens for which no vaccine exists, no matter how much research was thrown at them. While vaccines can protect us from dozens of infections, there are some bugs that just won't cooperate, for example, herpes simplex, HIV/AIDS, norovirus, Lassa fever, malaria, and hepatitis C.
4. What happens if no vaccine can be found?
Now, the options become limited (and worse):
- Containment has been used to prevent epidemics but Wuhan has already escaped. Too late.
- Like Zika, some pathogens just do not have "what it takes" to infect enough people to cause a pandemic. Viruses can mutate in a way that makes them either more or less infective to humans. If they become less likely to infect humans the pathogen can't efficiently spread and there will be no pandemic. But there's a big difference between Zika and Wuhan – Zika is transmitted by mosquitos while Wuhan is readily passed from person to person. Zika was not.
- New drug discovery – a time-tested, but lengthy process – has certainly been successful in providing game-changing antiviral drugs. For example, while there is no vaccine for herpes, HIV/AIDS, or hepatitis C (HCV), herpes can usually be controlled with acyclovir, HIV/AIDS drugs have been developed that are so potent that they shut down HIV replication and restore the immune systems of people who are infected, and hepatitis C can now be cured about 95% of the time. But it is time that is the problem.
Hepatitis C was discovered in 1989, but it took 22 years for the first two direct-acting antiviral drugs to hit the pharmacy and neither was any good. There are now a series of drugs that cure the infection called polymerase inhibitor. The first, Solvadi, wasn't approved until 2013 – 24 years after the virus was discovered, and this with almost every pharmaceutical company conducting HCV research projects. I led one of them at Wyeth. The campaign against HCV, like HIV, was a phenomenal success story, yet it still took a quarter of a century to get from the lab to the pharmacy.
The timeline for HIV/AIDS was a bit better, but it still not great. It took 14 years from the discovery of the virus (1981) until the approval of Saquinivir – the first HIV protease inhibitor, despite a massive global effort. Saquinivir became the first drug to make up "HIV cocktails," and it is no coincidence that 1995 was the first year that AIDS deaths began to drop.
Bottom line: Antiviral discovery programs led to unparalleled success for HIV and HCV, but it not going to help with a rapidly spreading new pathogen (4,5).
Conclusion/Prediction
The best cutting edge research, such as we are seeing with Wuhan and saw previously with HIV and HCV, can still fail or it can succeed. But even if everything goes right it will take far too long to have an immediate impact on a newly emerged pathogen that spreads easily.
Drug and vaccine development is slow going and there is only so much that can be done to speed it up. Even if Inovio really does have a vaccine ready to test in 16 weeks, the clinical trials required to determine if it works, and, if so, at what dose, will probably take a year, maybe more. Then figuring out how to grow enough of the vaccine to protect the world will probably take years.
There is no quick fix here. We need the best science, a lot of luck, and maybe a little cooperation from the virus. In the absence of a pleasant surprise, is unlikely that Wuhan will be under control anytime soon. But on a positive note, from what I'm reading, the prospects for a vaccine aren't bad.
NOTES:
(1) If you don't believe that vaccines are medical miracles, just skip this article and save both of us time.
(2) By contrast, in 1984 a bitter feud erupted about who first discovered HIV. Do not invite Luc Montagnier (Pasteur Institute) and Robert Gallo (National Cancer Institute) to the same party. The war between the two was vicious. It even got its own chapter in the book "Great Feuds in Medicine."
(3) Although Chinese scientists may have fully cooperated that does not necessarily mean that the Chinese government did. There have been news reports like this, which indicate that government officials tried to hide the news of Wuhan at the beginning of the outbreak.
(4) There is one exception, but it's a bit of a long shot. Although most antiviral drugs are specific for the virus they are intended to treat there are cases where some drugs that are effective against multiple viral infections. It is possible that a drug or combination of drugs already exists that would work against Wuhan. Universities and drug companies are already examining this option.
(5) A recent article in the Los Angeles Times suggested that Wuhan was as contagious as the 1917-18 Spanish flu, which infected 500 million people worldwide, killing 50 million.


