In medicine, the diffusion of innovation occurs over years. I have seen laparoscopic abdominal surgery (minimally invasive surgery) replace open surgery over 3 or 4 years in my clinical lifetime. The same for repairing aortic aneurysms with stent-grafts and correcting arterial blockages in the leg with stents; both have supplanted open surgical repair significantly. On the other hand, some innovation languishes. Repairing the carotid artery with stents rather than open surgery was anticipated to replace surgery by the late '80s. It still accounts for only 10% of treatment. This current paper looks at the adoption of dexamethasone in the treatment of COVID-19 in Australia.
Background
A preprint of the RECOVERY study was published on June 22nd. It demonstrated that dexamethasone, a commonly used steroid, could reduce the length of hospitalization and mortality for patients with COVID-19, especially those requiring mechanical ventilation. You can find our coverage here. Before that time, the published guidelines in Australia recommended against the use of dexamethasone. The peer-reviewed paper was published in the New England Journal of Medicine (NEJM) on July 17th.
The authors had access to a dataset of most patients with laboratory-confirmed COVID-19 in Australia's intensive care units. They wanted to know how quickly care changed in relation to posting the article's preprint and publication.
The Study
Four hundred sixty-one confirmed patients were cared for between the end of February and middle November of this year in Australia's ICUs. Frequently they were male, overweight, 60-ish, and short of breath. About a third were placed on ventilators upon admission, 53% sometime during that ICU stay. Prior to the preprint, those demographics were "more often male, leaner," more often on mechanical ventilation, and receiving hydroxychloroquine more frequently than remdesevir. Hospital stay was reduced, but mortality changed very little over the period.
Here is one picture is how physician-directed care changed in relation to the publication of the RECOVERY trial results.
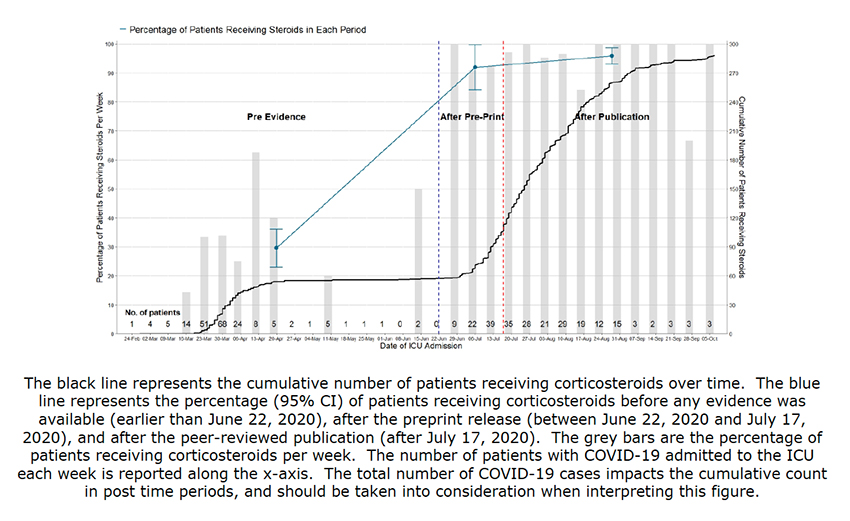 As you can see, there was a dramatic, immediate increase in the use of dexamethasone. Corticosteroid use increased from 29.5% to 92% with the preprint posting with a further small bump up (96%) with publication in NEJM. The increased use was similar for all ICU patients, irrespective of their ventilator needs, and for all size hospitals and ICUs. Physicians jumped on this treatment with both feet.
As you can see, there was a dramatic, immediate increase in the use of dexamethasone. Corticosteroid use increased from 29.5% to 92% with the preprint posting with a further small bump up (96%) with publication in NEJM. The increased use was similar for all ICU patients, irrespective of their ventilator needs, and for all size hospitals and ICUs. Physicians jumped on this treatment with both feet.
It remains unknown why physicians changed so quickly, but there is no doubt that they did. Dexamethasone is cheap, readily available, and has been used for years, especially in intensive care settings – familiarity and availability. And to be honest, the novel coronavirus had taxed on conventional treatments; we were trying everything because nothing seemed to help in these dire situations.
That has changed, and we now have protocols and approaches that work better, overall outcomes are improving. As with all things COVID, the sources of innovation and the speed of the diffusion were more revealed, and in this instance, accelerated. Other researchers will have to look for the reasons underlying why we quickly grasp on to some medications or techniques and let different approaches languish.
Chart Nerds Take Note
I apologize in advance to those who are not obsessed with data visualization. You can stop reading here. For those of you continuing, the study's graphic has so many visual faults that should be called out. The most significant error is that blue line showing steroid use in the three periods – it plots interval data as continuous, making the change seem gradual and continuous rather than abrupt. The black line representing cumulative cases adds little, except visual drama – even the authors write that it should be interpreted with caution. In short, the lines do not tell the story well. The horizontal guidelines add clutter, not clarity. And while those vertical lines separating the pre-evidence, preprint, and peer review periods work, simply shading the background with three different colors would have been, to my mind, more effective.
Source: Rapid Translation of COVID-19 Preprint Data into Critical Care Practice American Journal of Respiratory and Critical Care Medicine DOI: 10.1164/rccm.202009-3661LE




