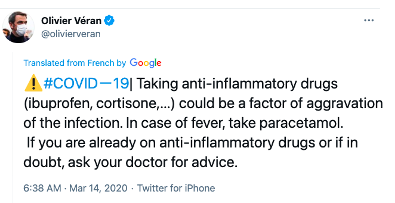
There has been considerable speculation that NSAIDs might be harmful to people who are suffering from the aches and pains of a COVID infection. Back in March Olivier Véran, the Health Minister of France tweeted the following:
In response, the European Medicines Agency stated that the was "no scientific evidence" that the use of NSAIDs was harmful:
"When starting treatment for fever or pain in COVID-19, patients and healthcare professionals should consider all available treatment options including paracetamol and NSAIDs."
Britain's National Health Service went the safe route by taking both sides:
"There is currently no strong evidence that ibuprofen can make COVID-19 worse. However, until we have more information, people should take [Tylenol] to treat the symptoms of coronavirus, unless they have been told by their doctor that paracetamol is not suitable for them."
Clear as mud, right?
Two large cohort studies (1) published by Angel Wong, Ph.D., and colleagues at the London School of Hygiene and Tropical Medicine in the Annals of Rheumatic Diseases may go a long way to clearing the mud.
The group examined reported results from two studies between March and June 2020:
Study 1 included 500,000 users of NSAIDs (for any reason) and more than 1.9 million non-users, both from the general population, and compared the COVID death rate in the two groups.
Study 2 included more than 1.7 million people with rheumatoid arthritis or osteoarthritis, ~10% of whom had prescriptions for NSAIDs. Again, the COVID death rate of the two groups was compared.
Results:
Study 1: There was no difference in the death rate in NSAID users and non-users.
Study 2: The NSAID users were 22% less likely to die from COVID. It's not clear whether this result is real or not. It's a little difficult to believe that NSAIDs protected people with arthritis from COVID but did not do so in the general population. This result is probably a statistical artifact (3). The authors concluded:
We found no evidence of a harmful effect of routinely prescribed NSAIDs on COVID-19 related deaths. Risks of COVID-19 do not need to influence decisions about the routine therapeutic use of NSAIDs.
Angel Wong, Ph.D.
While these studies seem reassuring it does not address several issues:
- Although the death rates were the same there is no information about the severity of disease. It would be interesting to know whether there was a difference in hospitalization rates in the two groups.
- The issue of whether to take NSAIDs either before or after being vaccinated is far from clear. It is not addressed in the studies. The input from the CDC, which suggests that you "talk to your doctor" about what medicine to use, is a useless cop out.
Although the picture of the role of NSAIDs in controlling symptoms from the disease is not yet complete the Annals of Rheumatic Diseases study should provide some comfort for the millions of people who are suffering from COVID and actually want a useful medicine (2) to help them get through the aches, pains, and fever of this awful, mysterious disease.
NOTES:
(1) For an excellent discussion of the relative usefulness of different types of studies see this from my colleague Alex Berezow.
(2) Tylenol can reduce a fever, but is close to useless in treating different kinds of pain.
(3) Or it could be related to some rheumatoid arthritis patients being on disease-modifying immune suppressants. It might be interesting for them to separate the RA and OA patients and see if there is anything there.