It took just my first MBA course on health systems to realize how provincial was my vantage point for all of my cosmopolitan ways. So before we explain away the differences in these statistics as just shoddy reporting, let us suspend our pre-judgments.
COVID-19 in India
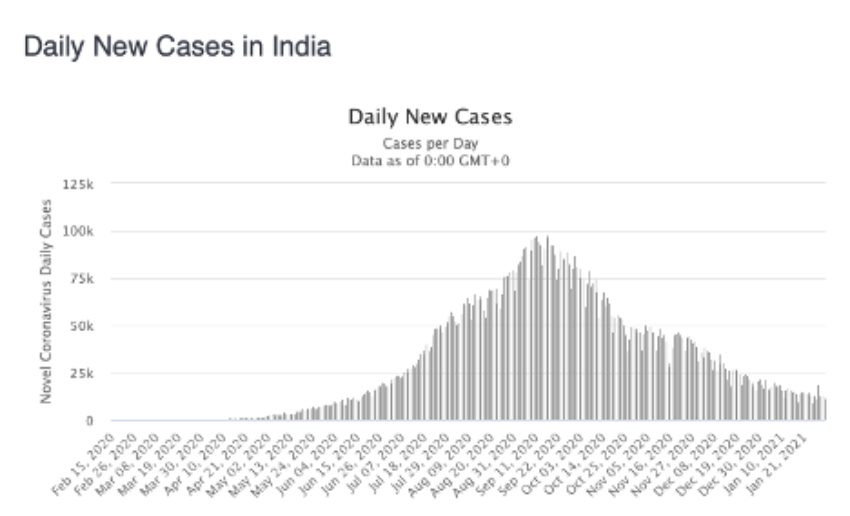 https://www.worldometers.info/coronavirus/country/india/
https://www.worldometers.info/coronavirus/country/india/
As you can see, daily new cases are down and by a lot. With a peak in September of 100,000 a day, it is now 10-fold lower. And here is a comparison with the US, from Johns Hopkins
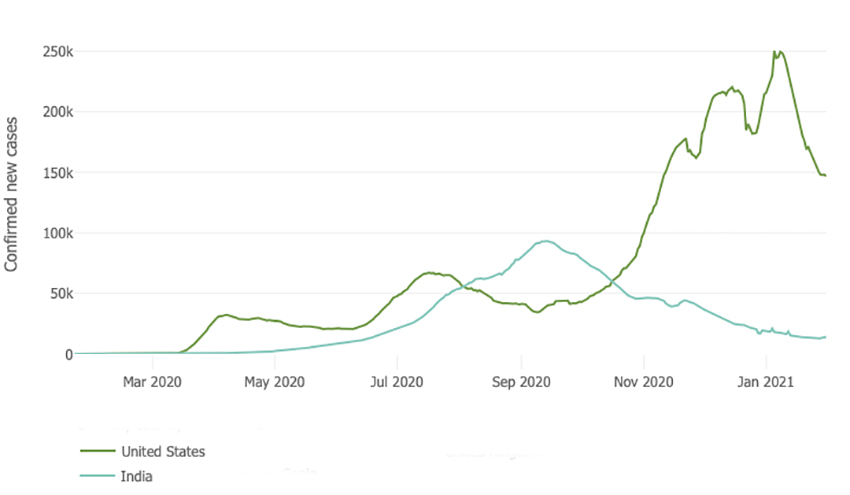 So I think it is fair to say that India is doing something different. Let’s begin with lockdowns. In March, India locked-down in what is described as a “draconian” way – public transport suspended, purchases limited to food, medicine, and cleaning supplies; and I am pretty sure there is no DoorDash or Amazon Prime available.
So I think it is fair to say that India is doing something different. Let’s begin with lockdowns. In March, India locked-down in what is described as a “draconian” way – public transport suspended, purchases limited to food, medicine, and cleaning supplies; and I am pretty sure there is no DoorDash or Amazon Prime available.
India’s built structure, testing, climate, and deaths
India is home to five of the 20 most dense cities; Mumbai is first with a density of 77,000 people per square mile; by comparison, our densest city, New York, has 27,000 people per square mile. A substantial percentage of those citizens, in both countries, live in what we would call in India slums (33%) and that we refer to here as high poverty neighborhoods (in New York City, the estimate is 25%). In any case, social distancing is more aspirational than real.
As it has been here, testing has been problematic, with much back and forth about the number of tests and their sensitivity. As reported in Science Magazine:
“Studies in August, for example, found antibodies in 41% of residents of Mumbai’s slums, compared with 18% elsewhere in the city. “Many dense pockets that can be easily infected have [likely] already been infected…”
“Malaria, typhoid, dengue fever are all endemic in India. People with robust immune systems are more likely to survive here in the first place, Shah says. Plus, more than half of the population is under age 25. They're less likely to die of COVID and more likely to get it asymptomatically. But India's climate and demographics have not changed during the pandemic, and the drop in cases here has been recent.” Lauren Frayer, NPR
The climate is different in India, more tropical in the South, more temperate, like the US, in the North. But as stated, the climate has not changed suddenly. India's people are relatively young; the over 65-year-olds account for only 6.5% of the population compared with 20% in Europe or 17% in the US.
Deaths are problematic; most Indians die at home without the benefit of having those death categorized. Deaths among those over age 85 are lower in India, perhaps due to “survivorship bias,” a fancy way of saying only the strong survive. (This would mesh nicely with my belief that American healthcare keeps many frail people alive, which is a good thing, overall). But deaths among 40 to 50-year-olds were 9% in India, four-fold greater than in the US. Why? One researcher suggested, “There is a lot of hidden diabetes and hypertension in the country.”
Is this herd immunity?
There is increasing speculation that India’s cities' high density, the real inability to social distance despite mandates, and the far greater incidence of asymptomatic cases in the slums all have made for herd immunity. That remains to be seen. The virus seems to have been more “concentrated” in the urban area rather than India’s rural areas, much like the early US experience. But those numbers are up in the air.
“The national epidemic is a “figment of statistical imagination. There are 100 or more small epidemics in different states and cities, rising and falling at different times.”
T. Jacob John, former head of Virology, Christian Medical College
Vaccination
India has launched as ambitious a vaccination program as the US, hoping to vaccinate 300 million by July. Like the US, the vaccine-hesitant are more than a speed bump, with 40% of physicians stating that they will wait and see about vaccination. Bloomberg reports that unlike the US, where people are waiting in frustration, only 56% of those who are eligible are coming forward to be vaccinated in India.
There is another aspect to vaccination that our nationalist point of view overlooks or minimizes. It is providing vaccines globally, especially to the many countries that cannot afford the two currently approved in the US. China has been waging a war of “vaccine diplomacy” for many months, rolling out a vaccine from Sinovac. It has encountered some difficulties of late as Brazilian studies show its efficacy at just over 50% compared to earlier studies touting a 78% efficacy. (Whether that matters is discussed more in-depth here.). But India has been the vaccine supplier to most lower-income countries for a very long time providing 70% of the vaccines distributed.
The Serum Institute, one of India's two powerhouse producers, has given away millions of doses to the countries surrounding India, doses of the Astra-Zeneca vaccine, the one being used by the EU. It has set aside production capabilities to make an additional 1 billion doses this year. It will produce another 1 billion doses of the Novavax vaccine – all these vaccines targeted to low and middle-income countries.
Sources: India eyes global vaccine drive to eclipse rival China Financial Times
India Has Plenty of Coronavirus Vaccines But Few Takers Bloomberg
India’s COVID-19 cases have declined rapidly—but herd immunity is still far away, scientists say Science Magazine
India: has the Covid pandemic started to burn itself out? Financial Times




