The title here refers to a saying among surgeons. It applies not only to our reputation, how others view us but to how we view ourselves, at least for a little while. A new study suggests that the sentiment behind the saying also influences our subsequent few medical decisions.
The study, published in Science, looks at the decision to perform a vaginal delivery or cesarian section – a binary choice that is important because that decision can impact infant and maternal mortality. There are any number of variables that go into making the call, all balancing the well-being of both mother and infant, both short and long term. For the study and understanding what the researchers found, we can put those concerns to the side. As the researchers point out, “there is a lack of high-quality evidence” to guide physician decisions.
Researchers retrospectively reviewed of 20 years’ worth of electronic medical records involving deliveries, 86,000 in total, at two academic medical centers. There is no reason to believe that the means of delivery in the first patient will be determinate of the means of delivery of the next patient – over time, without a bias towards vaginal or cesarian delivery, the occurrences should be random.
Here is the question, if the first patient has a complication, will the physician be more likely to stay with the same mode of delivery, or will they think perhaps the alternative approach would be safer? The term the researchers use is a “win-stay/lose-shift” heuristic. The data set included 26,000 cesarian sections, 60,000 vaginal deliveries. The only significant difference in the two groups was that those women undergoing cesarian section were slightly older, 30, and slightly more likely to experience complications. The underlying assumption is that the only thing changing is the physician’s perception of what might be best – are we only as good as our last decision (case)?
- Irrespective of whether the prior case was a vaginal or cesarian delivery, a complication increased the probability that the next patient would have the opposite mode of delivery by about 3.4%—an admittedly small number, but one with statistical significance.
- When the prior delivery had no complications, the probability of the following patient having the same type of delivery was roughly 78%.
- These effects quickly faded and were not seen in the subsequent patients after the dyad.
So, there seems to be some evidence that the “win-stay/lose-shift” heuristic may be at work in this situation. But does it confer a clinical advantage – does switching help or harm the patients? It seems that, unfortunately, it does not.
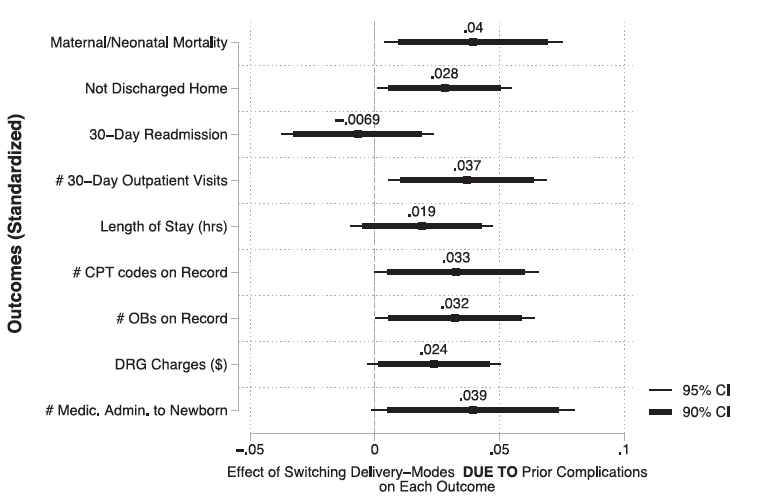
The figure shows in the attempt to avoid the complications in the first patient; there were still complications in the next. Again, the percentages are small, but increased post-delivery care in the hospital or outpatient seemed significant, as does maternal and neonatal mortality.
One must be extremely careful in interpreting this data and not pushing or contorting the data into a causal link. It is from one health system, in one state, with important information about the facts at the time unavailable or left out. That said, it does suggest that physicians, like all of us, respond to our recent experiences. The researchers suggest that this heuristic is found more frequently in the US because we do not use midwives who do not have the scope of practice to switch to a cesarian section or because of the invisible bias of malpractice litigation on physician thinking.
"…as an implication for research, this study highlights the importance of the physician as an individual—one with beliefs, preferences, and experiences rather than simply as a neutral provider of care—in influencing patient outcomes."
Permit me to speculate and suggest that one advantage of systems involving midwives is the consistency of care. Obstetrical on-call is challenging; a busy practice will have deliveries at all times of the day and night; and that wears upon physicians, especially as they age. Increasingly obstetrical practices utilize the physician-on-call rather than a woman’s specific obstetrician for their delivery. They also make use of hospital-based “laborists,” who provide 24-hour delivery coverage. Could it be that not having a long-term relationship between physician and patient also can affect care? I think it is one more variable that needs to be considered when you are only as good as your last case.
Source: Heuristics in the Delivery Room Science DOI: 10.1126/science.abc9818

