Perhaps. A new study in Science suggests a very high prevalence of the Epstein-Barr virus in patients with Multiple Sclerosis (MS). This strong evidence may aid those suffering from MS and give us all a better sense of how endemic infections may have long-term consequences that we are slow to recognize because of the long delay between infection and symptoms.
A bit of background
MS results in the demyelination of nerves in the central nervous system; its cause remains unknown. Myelin is a fatty-protein mix that wraps around our nerves like insulation, allowing the electric signal of the nerve to be conducted more quickly. For an unknown reason, some individuals' immune systems attack the myelin, “shorting out” the signal and resulting in fatigue, difficulties with walking talking, unsteadiness of gait, and generalized weakness. As with other chronic diseases, MS does not “happen” suddenly. There is an asymptomatic (sub-clinical) period as myelin is destroyed. A non-specific biomarker of this process, neurofilament light chains (Nfl), can be found in the blood of patients who subsequently develop MS years later.
The Epstein-Barr virus (EBV) has infected upwards of 95% of adults, most remaining asymptomatic and not reaching clinical identification. Mononucleosis, the “kissing” disease of my youth, is caused by EBV. It is a member of the herpes family and “after infection persists in a latent form in B lymphocytes throughout the life of the host.” Like herpes, it is never cleared from the body. Although it has been long suspected, the difficulty of calling EBV the “causative” agent of MS is that most people with EBV do not develop MS. So when we speak of EBV as a cause of MS, recognize that it is necessary, but not sufficient – there is no causative smoking gun
The study
Researchers made use of data collected over 20 years from the US military. The military required screening for HIV for all active-duty members, and those samples, 62 million from 10 million individuals, have been maintained since collection. The researchers found that 5.3% of samples were negative for EBV at the time of collection, and the medical events for these active-duty individuals could be followed over time. They identified 801 cases of MS where their EBV status was known to be negative before the onset of MS, a median of 10 years later. They used two randomly selected active-duty personnel matched to the age, gender, race, branch of service, and dates of blood collection of those 801 MS cases as their control.
At the baseline, 35 individuals with MS were seronegative for EBV. All but one became infected with EBV, and all were seropositive before the onset of MS. By contrast, in the controls without MS, only 57% became seropositive during the interval. Let us put this in the terms that garnered the headlines. If you developed an EBV infection, you were 32 times more likely to develop MS than if you remained seronegative. That is a very big number. By comparison, the risk of developing lung cancer among heavy smokers is 21-fold.
The researchers performed additional tests to strengthen their argument.
- Cytomegalovirus (CMV) is another member of the herpes family, transmitted through saliva like EBV and found in very similar socioeconomic and racial groups. Seroconversion from CMV negative to positive was no difference between those developing MS and those not suggesting that “behavioral, environmental, or personal characteristics” were not a factor.
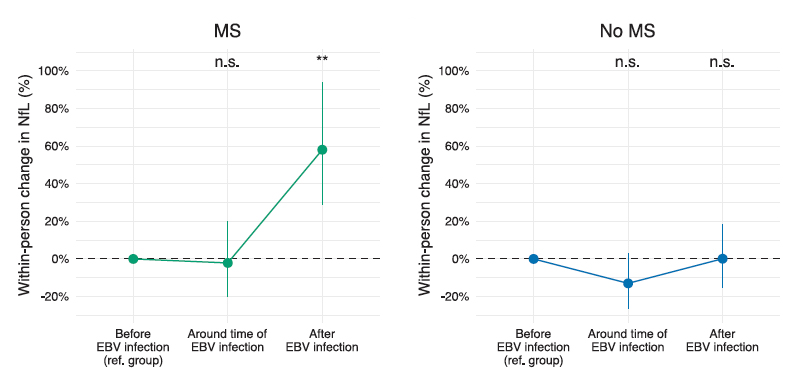
- Levels of NFL, that non-specific biomarker of demyelination were similar between those developing MS and the controls “before and around the time of EBV infection but increased after EBV infection…indicating that EBV infection preceded not only symptom onset but also the time of the first detectable pathological mechanisms underlying MS.”
- They took 30 of their MS serum samples with their matched controls and searched for evidence of other viruses based upon antibodies. They looked at serum samples just before and after the onset of MS symptoms. The patterns of viral antibodies were again similar for both MS patients and controls in those two periods, with one exception, EBV antibodies in MS patients. This rules out the idea of reverse causation – that an immune dysfunction leads to the increase in EBV infections
“The addition of MS to the list of diseases that an EBV vaccine could target strengthens the rationale to accelerate ongoing research…”
In their discussion, the researchers suggest that an EBV vaccine and the use of antivirals [ARE THERE ANY USEFUL ANTIVIRALS FOR EBV?] could alter the onset and course of MS. For the rest of us, this study shows that infections, specifically viral infections, may affect our health well past the time of our acute symptoms. We see this in individuals being diagnosed as having “Long COVID.” We have a great deal more to learn about MS and Long COVID, but we should be struck by their patterns. Many microbes set up their homes within us, including the gut microbiome. Those residents may well provide us with benefits, but sometimes they may create chronic illness – it is only a matter of how they affect us that makes them beneficial or a pathogen.
Source: Longitudinal analysis reveals high prevalence of Epstein-Barr virus-associated with multiple sclerosis Science DOI: 10.1126/science.abj8222

