
Although shared long before Citizen Kennedy became Secretary Kennedy, the following tweet has not aged well. More important, it demonstrates how a kernel of truth can be wrapped in misdirection by our current Secretary of Health and Human Services, raising concerns that should cut across partisan lines.
To understand both the kernel of truth and the misleading wrapper, and to know how Citizen Kennedy distorted the truth, we must first grasp the devastating disease Gardasil helps prevent: cervical cancer.
Cervical Cancer and Human Papillomavirus (HPV)
The cervix is the lower, narrow portion of the uterus connecting the uterus to the vagina, the gateway between the uterus and the outside world. The endocervix forms the canal leading into the uterus, while the exocervix is the outer surface of the cervix. The transformation zone where these areas merge is where most cervical cancers originate. These cancers typically develop gradually as normal cells become “precancerous” cells. In some cases, these precancerous changes resolve without treatment; in others, they progress over time, eventually developing into cervical cancer.
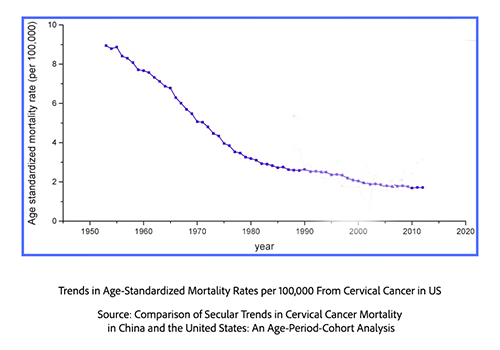 The mortality from cervical cancer has been in decline since the early 1900s, but as this graphic demonstrates, the survival rate began to improve precipitously in the 1950s. That improvement was due to the pioneering efforts of a Greek immigrant physician, Georgios Papanicolaou. Working at NYU and Cornell, he discovered that reproductive cycles could be tracked through vaginal cell smears and that microscopic examination of cervical cells could distinguish normal from malignant changes. Although initially overlooked, fifteen years later, in 1943, he co-published Diagnosis of Uterine Cancer by the Vaginal Smear, confirming that simple cervical swabs could reliably detect cancerous and precancerous cells. This technique, the Pap smear, is perhaps the most successful screening test for cancer, particularly in identifying cancers of the exocervix, less so for the endocervix. Because of this difference in screening, there has been a dramatic decrease in exocervical cancers and a persistent presence in endocervical ones.
The mortality from cervical cancer has been in decline since the early 1900s, but as this graphic demonstrates, the survival rate began to improve precipitously in the 1950s. That improvement was due to the pioneering efforts of a Greek immigrant physician, Georgios Papanicolaou. Working at NYU and Cornell, he discovered that reproductive cycles could be tracked through vaginal cell smears and that microscopic examination of cervical cells could distinguish normal from malignant changes. Although initially overlooked, fifteen years later, in 1943, he co-published Diagnosis of Uterine Cancer by the Vaginal Smear, confirming that simple cervical swabs could reliably detect cancerous and precancerous cells. This technique, the Pap smear, is perhaps the most successful screening test for cancer, particularly in identifying cancers of the exocervix, less so for the endocervix. Because of this difference in screening, there has been a dramatic decrease in exocervical cancers and a persistent presence in endocervical ones.
The next leap in the understanding of cervical cancer came from German virologist and later Nobel Laureate Harald zur Hausen, for the discovery that most cervical cancers were caused by human papillomavirus. [1]
His initial discovery of the Epstein-Barr virus (EBV) in a type of lymphoma helped initiate the field of viral-caused cancer, onco-virology. Dr. Zur Hausen initially identified a strain of human papillomavirus (HPV) in genital warts and subsequently in cervical cancers. Human papillomavirus (HPV) is a group of more than 200 viruses, many of which spread through intimate contact, i.e., sexual intercourse.
Low-risk strains can cause genital warts, while high-risk strains, e.g., HPV 16 and 18, can cause cancers of not only the cervix but of the anus, throat, penis, vagina, and vulva. Nearly all individuals who are sexually active have been infected at some point, and virtually all cervical cancers are caused by HPV.
Normally, the immune system clears HPV infections within a year or two. But when high-risk types persist, they disrupt infected cells' growth and communication, leading to precancerous lesions and, eventually, cancer, especially in areas like the cervix. Typically, precancerous lesions develop 5 to 10 years after infection, remaining asymptomatic for decades until transforming into cancers. Infection with aggressive strains like HPV 16 or 18, smoking, early sexual activity, multiple sexual partners, and a weakened immune system can all contribute to the risk of cervical cancer.
Fortunately, medical science has equipped us with a powerful tool to combat HPV and its cancerous consequences: the Gardasil vaccine.
Gardasil
Gardasil 9, the HPV vaccine, protects against infection from nine HPV types, including the seven types that cause most HPV-related cancers and two strains causing genital warts. The vaccine consists of virus-like particles, not genetic material, mimicking 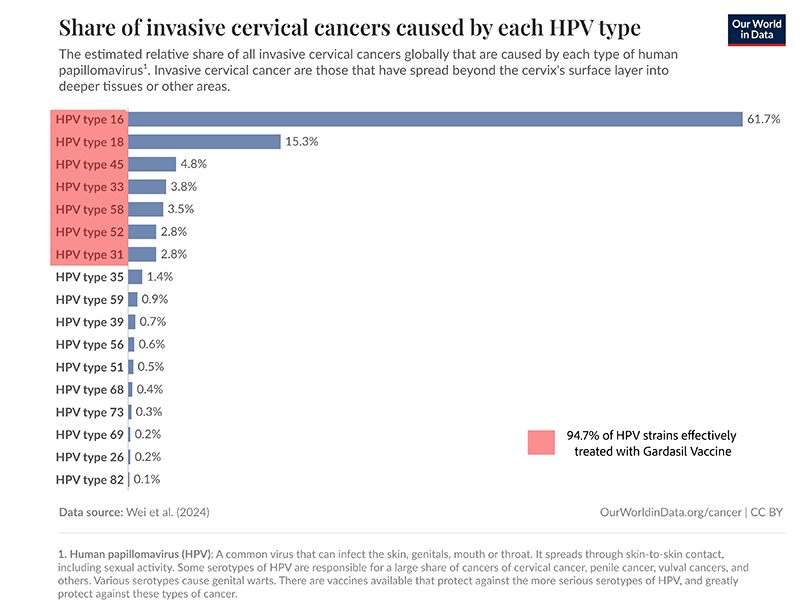 the proteins found on the surface of the HP virus. The vaccine is highly immunogenic, providing significant protection, estimated at 90% from cervical cancers.
the proteins found on the surface of the HP virus. The vaccine is highly immunogenic, providing significant protection, estimated at 90% from cervical cancers.
Extensive research confirms that HPV vaccines are highly safe. A Cochrane review found no increased risk of serious adverse effects. Although slightly more deaths occurred among vaccinated women over age 25, none were linked to the vaccine. With “more than 135 million doses” administered in the US, the CDC’s Vaccine Adverse Event Reporting System (VAERS) safety data show that most side effects are mild, such as injection site reactions, dizziness, fainting, nausea, and headache. Apart from fainting, which is common across all adolescent vaccines, no serious adverse events have been confirmed at higher-than-expected rates. Severe allergic reactions like anaphylaxis are exceedingly rare.
A study of nearly 500,000 Scottish women, published in the Journal of the National Cancer Institute, found no cases of invasive cervical cancer among those vaccinated with the HPV vaccine at ages 12 or 13, regardless of the number of doses. But age of vaccination matters.
“The girls that didn’t develop any cancer were vaccinated before becoming sexually active.”
- Kathleen Schmeler, MD, Professor of Gynecologic Oncology, MD Anderson Cancer Center
For women vaccinated later, between ages 14 and 22, with three rather than two doses, the incidence of cervical cancer dropped significantly compared to unvaccinated women (3.2 per 100,000 vs. 8.4 per 100,000).
 Despite the vaccine’s proven effectiveness and strong safety record, Gardasil has been met with resistance. It epitomizes the paradoxical response that highlights the complicated terrain of vaccine acceptance and public trust that Secretary Kennedy disingenuously engages.
Despite the vaccine’s proven effectiveness and strong safety record, Gardasil has been met with resistance. It epitomizes the paradoxical response that highlights the complicated terrain of vaccine acceptance and public trust that Secretary Kennedy disingenuously engages.
Acceptance and Hesitancy
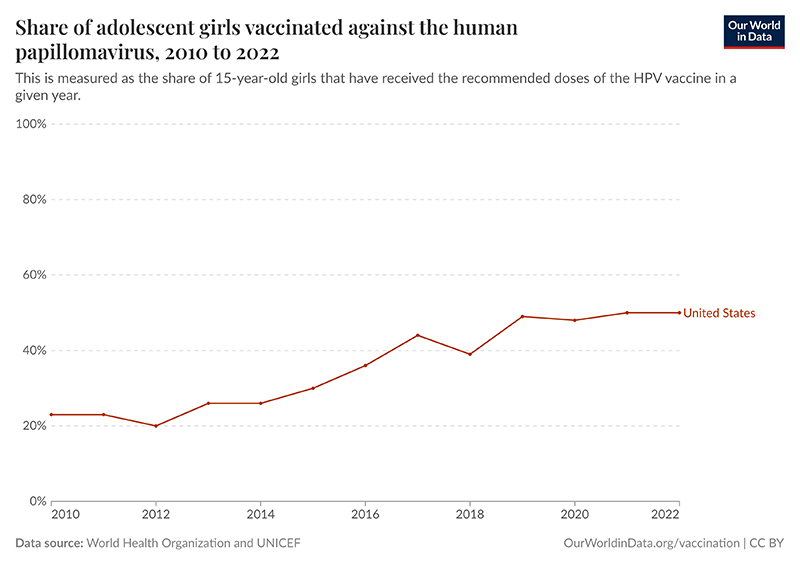
Vaccination is part of in-school care in Scotland, resulting in very high vaccination rates. In Denmark, the vaccination rate is 89%, almost in line with the global goal of a 90% vaccination rate. In the US, the current rate is 50%.
In addition to greater vaccination hesitancy brought on by the COVID-19 pandemic, the HPV vaccine raises concerns among parents because it protects against a sexually transmitted infection. Multiple studies have shown that parents in the US, as well as more culturally conservative countries, will prioritize cancer prevention over concerns about sexual activity. However, despite early sexual activity being relatively common by age 16, both parents and providers are hesitant to ascribe sexual activity to younger adolescents, contributing to lagging vaccination rates. More important, immunization is most effective before the onset of sexual activity.
In a commentary in JAMA Network Open on the safety of HPV vaccination, the authors note,
“Studies have shown that while individuals trust medical professionals for health information, a growing number are turning to the internet for first and second opinions about HPV, HPV vaccines, and HPV-associated cancer. … unfortunately, information warning about the HPV vaccine is often based on half-truths or is completely baseless.”
This brings us to citizen, now Secretary Kennedy’s tweet about a rising risk of cervical cancer from an HPV vaccination.
Gardasil is not 100% effective, and its efficacy declines with the timing and completion of the vaccination series (two doses for those 9-14, three doses for those 15-26). As a result, continued screening with Pap Smears remains a necessary part of surveillance. Full stop.
The population data on “vaccinated age groups” Secretary Kennedy alluded to reflects aggregate numbers. While it is easy to demonstrate Gardasil’s efficacy for an individual, a significant sample size is required to demonstrate efficacy at the population level. At least 70% of at-risk individuals must have been vaccinated, which is not true in the US. Moreover, since vaccination is not wholly protective, cervical cancer rates increase when subsequent Pap smear screening is reduced. The mathematical minimum is 80% screening to avoid increased cervical cancer in a population with vaccination rates similar to that in the US – and our current rate is about 70%
The video alluded to by Secretary Kennedy, from his former work at the Children’s Health Defense (CHD), reports a rise in cervical cancer rates among UK women aged 20–24. Still, the 2018 analysis they cite attributed the increase to more women being screened at age 24.5, not to vaccine failure. Moreover, the study never documented vaccine status. [2]
CHD goes on to suggest that vaccination increases the cancer risk.
“For example, a 2015 study found that vaccinated young adult women had a higher prevalence of high-risk HPV types other than types 16 and 18, putting them at risk for more aggressive cervical and other HPV-related cancers.”
But, the cited study involves the initial quadrivalent vaccine, not the current version treating 9 HPV strains. After noting the 90% efficacy against the two high-risk strains then being treated, the researchers who performed that study wrote,
“One interesting finding was that vaccinated young adult women had a higher prevalence than unvaccinated women of high-risk types other than HPV 16 and 18, and thus are still at risk of cervical cancer and other HPV-related cancers. …The underlying causes for the increased prevalence of high-risk nonvaccine types we observed among vaccinated women cannot be determined from these data. However, we found that the association between vaccination and differences in prevalence of high-risk nonvaccine type infections was attenuated after adjusting for sexual behavior variables.” [emphasis added]
Secretary Kennedy's attack on the HPV vaccine echoes the same misleading tactics he once used against the MMR vaccine: weaving selective truths into a tapestry of fear. In Texas we are now reaping the vaccine hesitancy that Citizen Kennedy sowed over the last few years. Gardasil is not only safe and effective, it is a critical tool in preventing deadly cancers. By distorting the science, Secretary Kennedy risks undermining decades of progress in cancer prevention—and jeopardizing the very lifesaving public health efforts he is tasked to protect. If Secretary Kennedy truly wants to 'Make America Healthy Again,' he must start by rejecting the misinformation peddled by Citizen Kennedy—and by embracing the science that saves lives. Making America Healthy Again requires Keeping America Healthy.
[1] He was aided in his research by his wife, Ethel-Michele de Villiers, who, while not receiving a part of the Nobel, was at least credited by her husband with her contribution in his biography.
[2] The UK program for school-age girls was initiated in 2008, and the cohort included girls whose vaccination rate was about 70% and those slightly older, “catching up” with vaccination where the vaccination rate was about 50%.
George Papanicolaou (1883–1962): Discoverer of the Pap smear
Cervical Cancer Causes, Risk Factors, and Prevention National Cancer Institute
HPV vaccination: How the world can eliminate cervical cancer Our World in Data



