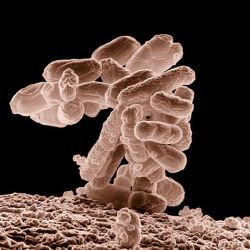
Clostridium difficile (C. diff.) colitis is a terrible infection involving the colon or large intestine. It produces watery diarrhea that can be so debilitating that you do not have the energy to get out of bed. It often results from taking antibiotics, not exactly precision medicine. Antibiotics have systemic actions, and along with treating the underlying infection, they alter our normal bowel flora, our microbiome. As the flora shifts, C. diff proliferates releasing the toxins that are responsible for much of the misery associated with C. diff. Infections (CDI).
CDI is not a small problem, there are close to 500,000 cases annually, and 100,000 of those patients (20%) develop recurrences requiring re-treatment. The estimated costs approach $4.8 billion annually. Now the most straightforward means to reduce CDI is to eliminate the use of unnecessary or incorrectly chosen antibiotics and good hygiene – washing your hands, cleaning surfaces. But sometimes you have no choice you need antibiotics. A paper entitled, Protection of the Human Gut Microbiome from Antibiotics, by Jean Gunzburg et al. published in the Journal of Infectious Diseases explores a possible way to make antibiotics safer.
Oral antibiotics that enter the colon cause the microbiome shifts that result in CDI. In some cases, oral antibiotics are not completely absorbed in the small intestine; while for parenteral (intravenous) antibiotics and to a lesser degree oral antibiotics they are secreted in the bile and find their way to the colon. Da Volterra, a French company, has developed a nonspecific absorbent activated charcoal that is delivered to the end of the small bowel, DAV132, that absorbs these drugs preventing them from altering the flora of the colon. Let's start with a few pertinent points. This is a safety and efficacy study, so the number of participants is small. And it is a study funded by Da Volterra, a French company, that produces this new protective agent.
Twenty-eight volunteers with given a five-day course of a fluoroquinolone, specifically Moxifloxacin (MXF), one of the drugs associated with CDI. Half of the volunteers acted as controls receiving MXF alone, the other half, the treatment group, received MXF and DAV132, the activated charcoal.
- There was no difference in the plasma levels of MXF in either group – this is important because it shows that the charcoal did not reduce the availability of the drug to the bloodstream.
- Fecal level of MXF were 136 micrograms/gm of feces in the control group, and 14 micrograms/gm in the group treated with DAV132 – this demonstrates that the charcoal was effective in reducing antibiotic entering the colon
- The microbiome of the colon was characterized by extracting and quantifying the DNA in the fecal samples, a standard technique. MXF decreased the diversity of the DNA (meaning that some bacteria had been eliminated) by 46%. For those taking MXF and DAV132, the diversity declined by only 3% - So the charcoal did afford protection, but that protection was incomplete.
- There were no ill effects from taking the DAV132 – so it appears safe.
Now the study itself points out that these findings are not clinically significant. We do not have any clinical evidence that DAV132 will reduce the incidence of CDI. And we have no information on how DAV132 could affect other medications we are taking. So there is a lot of work to do to get from this simple study to a clinically useful drug.
Source: Journal of Infectious Diseases, https://doi.org/10.1093/infdis/jix604