Some vaccines are one-and-done, like measles. Others are annual events, like the seasonal flu. There's new data as to where on that spectrum the COVID-19 vaccine lies.
Let’s start with some terms and background.
IgG – is a specific type of antibody and is the predominant antibody found in our blood. It is what provides our “immune” response, binding to the pathogen and enhancing the ability of our immune system’s cellular elements to engulf and destroy the invasive pathogen. They are formed by B cells in our bone marrow after being exposed to a foreign antigen – the COVID-19 virus or the mRNA vaccine-produced spike protein.
Neutralizing antibodies – These are a subset of IgG that develop somewhat later in the immune response. They can prevent the microbe, in this case, the COVID-19 virion, from attaching to a cell or entering a cell to replicate. They also can keep pathogens from changing their structure to “jimmy” the cellular lock.
IgG is our rapid response; the subset of neutralizing antibodies are the snipers.
The Pfizer vaccine, this is an Israeli study, like the Moderna, is very effective and creates high levels of IgG and neutralizing antibodies 7-14 days after the second dose. But there is evidence that the levels decline over time, especially in the immunocompromised and older age groups, whose immunity is aging along with the rest of their bodily functions.
The Study
The participants were all healthcare workers at a single hospital system who had blood samples drawn monthly before and six months after completion of their vaccinations. None of them were PCR-positive for COVID before immunization. Because testing for neutralizing antibodies is time-consuming and expensive, only a subset of the participants had that analysis done on their blood.
The study ran from December 2020 to July 2021, so Delta infections are in the mix. There were 4,868 initial participants; with completion of questionnaires, that was reduced to 3,808. There were 20 breakthrough infections for vaccine effectiveness of 99.5%. 26% of the cohort had neutralizing antibody data.
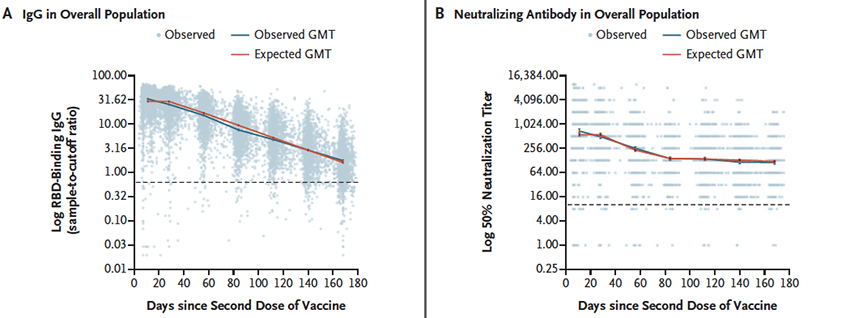
As you can see, both IgG and neutralizing antibodies declined over time – the overall IgG followed a linear, constant decline; the neutralizing antibodies declined over the first three months and then remained essentially stable. When stratified by age, the declines follow the same shape but were greater in those age 65 or greater. The same shape holds when stratified by gender, but males declined faster than females.
IgG levels were also reduced in those with co-morbidities and those who were immunocompromised. Neutralizing antibodies were also reduced in the immunocompromise but, interestingly, not in those with co-morbidities. Those characterized as obese, with a BMI of 30, had “significantly higher” neutralizing antibodies than their more svelte companions.
There are a few key findings:
Our immune response is a composite of the declining levels of IgG and neutralizing antibodies. The decline in these factors is more significant than seen in measles, mumps, and rubella – the one-and-done vaccines. [1] That is good evidence for the need for a COVID-19 booster and suggests that we might need a yearly tweak, just like for seasonal flu.
Neutralizing antibodies are thought to be the more protective of the two antibodies (the IgG is directed at the spike). That said, there is a changing correlation between IgG and neutralizing antibody levels. The correlation is greater early and diminishes with time as a result of their different rates of decline. Studies reporting only IgG levels as the proxy for our immune response depend on when titers are drawn. IgG is a good proxy early, not so good at 6-8 months.
Finally, other studies have shown that the IgG and neutralizing antibody levels that develop from infection-induced immunity are higher than those from vaccine-induced. The researchers suggest this may explain the differences in “breakthrough” infections from these two different immune stimulators. And yes, the immune response may be better after being infected, but the consequences of being ill are greater – it is not a tradeoff, and we needn’t condone COVID-19 “super spreader parties,” intended or not.
[1] Actually, measles, mumps, and rubella are given in two doses, usually separated by three years, but boosters are not necessary once that immunity is achieved.
Source: Waning Immune Humoral Response to BNT162b2 Covid-19 Vaccine over 6 Months NEJM DOI: 10.1056/NEJMoa2114583