
Fifty or so years ago a woman diagnosed with breast cancer was almost sure to be treated aggressively — with a radical mastectomy. That surgery involved removing, not only the affected breast tissue, but also the underlying muscle and many if not all of the nearby lymph nodes. Not only was that surgery disfiguring, it also caused various morbidities such as lymphedema (1) and difficulty in using the arm. More recently, of course, we have moved on and no longer need to take such draconian measures as often as before — we have a larger armamentarium of systemic treatments (e.g. chemotherapy) and more targeted radiation treatments.
Today, a woman presenting with an early stage breast lesion which has spread to some degree to nearby (sentinel) lymph nodes, could be treated with surgical excision of the tumor (a so-called lumpectomy) and removal of lymph nodes in the neighboring underarm area (axilla), followed by chemo and radiation. This removal of axillary lymph nodes still can put the woman at risk of significant lymphedema.
Dr. Armando E. Giuliano from Cedars-Sinai Medical Center in Los Angeles and colleagues investigated whether removal of axillary lymph nodes really improved survival in women who had been diagnosed with early breast cancer that involved the sentinel lymph nodes, and had been treated with lumpectomy, chemotherapy and radiation. What if only the sentinel nodes had been removed, and then chemo and radiation followed according to the usual protocol?
These researchers analyzed data from a phase 3 randomized clinical trial that assigned patients with clinical T1 or T2 breast cancer to receive lumpectomy, breast radiation, and chemotherapy and either axillary lymph node dissection or just sentinel node dissection. The participants were then followed for a median of 9 years. The results of their analyses were published in JAMA.
Participants in the study were women of about 55 years old; 436 were assigned to receive only the sentinel node dissection (SLND) and 420 received axillary node dissection (ALND). All had T1 or T2 primary breast cancers (refers to the size of the tumor), with 1 or 2 sentinel lymph nodes that were positive for tumor cells, but no evidence of distant metastases and no palpable axillary nodes. The majority had tumors that were hormone receptor positive.
The investigators determined that the overall survival rates 10 years post-surgery were basically the same for both groups, as was disease-free survival, as shown in the graphs below.
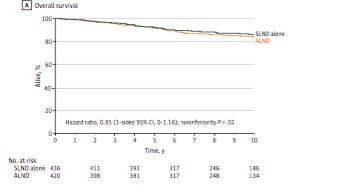
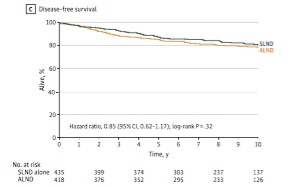
What these data tell us is that for women with these types and sizes of tumors, it made virtually no difference if only the sentinel lymph nodes were removed, compared to also removing the axillary nodes. So a woman falling into this category of tumor would be expected to do as well with just a lumpectomy followed by standard treatment as one who had more extensive node removal.
The authors concluded:
Axillary dissections are associated with considerable morbidity, and the results of this trial demonstrated that this morbidity can be avoided without decreasing cancer control. The long-term outcome of this study provides additional support that axillary dissection is not necessary for long-term disease control and survival for patients with positive sentinel nodes
1) Lymphedema is swelling of (usually) an arm or leg after lymph nodes near that limb have been removed. Protein-rich lymph fluid settles in the tissues rather than being drained by the lymphatic system. This can result in swelling, pressure, pain, and greater susceptibility to infection in the affected limb.



