While Americans were (sort of) celebrating the Fourth of July, the coronavirus kept raging on. Some relevant developments and analysis have occurred in the past few days that might shed a little more light on how the pandemic will unfold.
1) The coronavirus mutated to become more infectious. That sounds scary, but it doesn't appear to be. Not yet, anyway. The conventional wisdom posits an inverse relationship between infectiousness and virulence; i.e., if one goes up, the other goes down. In other words, milder diseases spread further than deadlier diseases. The corollary is that a new infectious disease should evolve to become less lethal. Though it intuitively makes sense (because a dead host can't spread the disease), it's not an immutable law. One study in songbirds showed that a bacterial disease got more virulent over time.
A new study published in the journal Cell shows that changing a single amino acid residue in the SARS-CoV-2 Spike protein (which binds the virus to cells) appears to have been sufficient to make the virus substantially more infectious. In early March, the old virus (D614) predominated globally; by late March, it largely had been replaced by the new virus (G614).
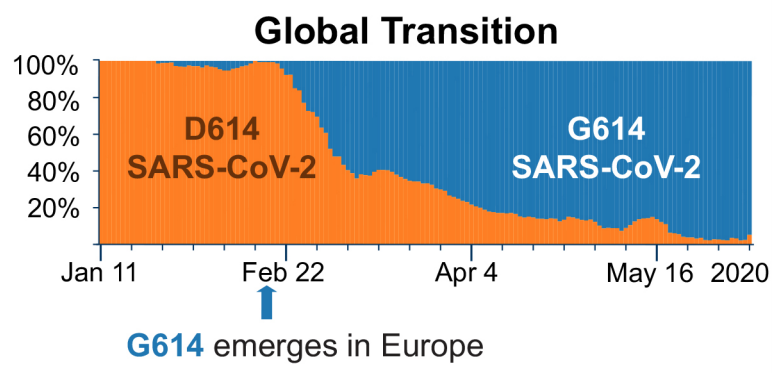
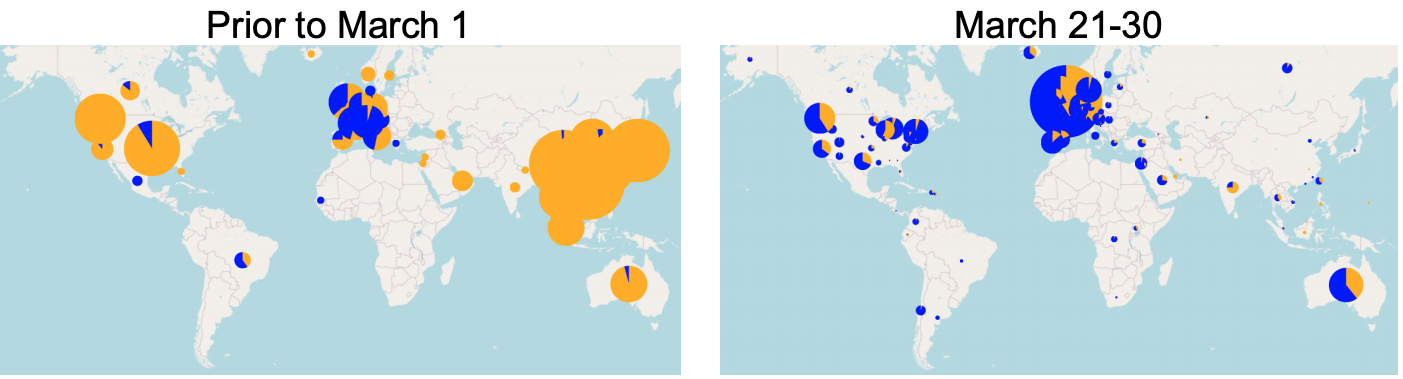
Source: B. Korber, et al. Cell 2020.
There is good news, however. The authors report that the virus has an overall mutation rate that is very slow. Even better, they found that patients who had recovered from a COVID-19 infection had antibodies that could neutralize the new virus. This would indicate that the efforts to design a vaccine have not been undermined by the mutation.
2) Though the mutation does not affect current vaccine efforts, a vaccine may not be the best solution. My colleague, Dr. Josh Bloom, and ACSH advisor Dr. Katherine Seley-Radtke penned an op-ed for the Baltimore Sun, explaining that an antiviral cocktail of drugs might prove to be the most successful approach.
There are at least three reasons for this. First, there are myriad viral infections -- from HIV to RSV -- for which there is no vaccine. Producing a successful vaccine is extremely difficult work, and if scientists aren't careful, they can manufacture one that actually exacerbates the illness rather than protects against it. Second, we still have no idea if coronaviruses elicit long-term immunity in humans. If they do not, then a vaccine becomes less attractive. Third, antivirals have a proven track record of success for some diseases, like HIV and hepatitis C. Thus, Drs. Bloom and Radtke believe that we should place our collective hope in an antiviral to fight COVID-19.
3) We don't have a good understanding of herd immunity to coronavirus. Contrary to what some people (and media outlets) believe, herd immunity does not mean that there will no longer be any transmission of the virus. Herd immunity instead refers to the proportion of people who must be immune in order to prevent outbreaks or epidemics. Traditionally, we determine a population's immunity to a virus by measuring antibodies, but there is now evidence that some people may have non-antibody immunity to SARS-CoV-2. (This is a part of the immune system known as cell-mediated immunity.) Antibodies may simply be one part of an incomplete picture.




