The researchers collected 205 nasopharyngeal swabs of all patients presenting to the Emergency Department (at NYU) over a week in March, who presented with symptoms consistent with COVID-19. They did both qualitative, but more importantly, quantitative testing, so that the patients’ outcomes could be linked to the amount of virus present, the viral load.
One hundred sixty-five patients were discharged and followed as outpatients; the remaining 40 were hospitalized. As you might expect, the discharged patients with younger and slightly more of the hospitalized patients were African American or Asian, with more co-morbidities – all within the narrative of the COVID-19 susceptible. Those being hospitalized had symptoms for five days, two days longer than those treated as outpatients.
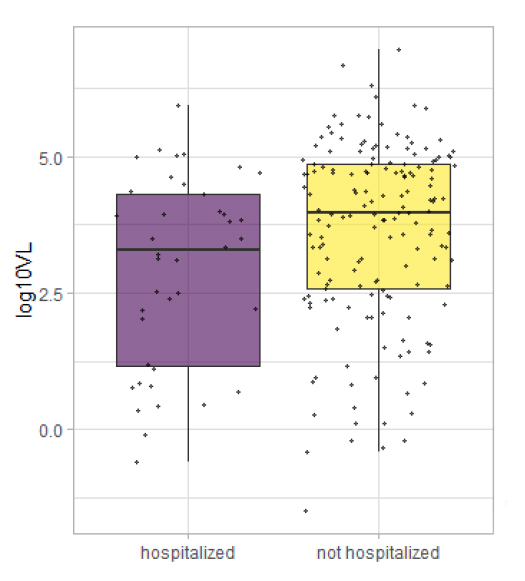 Here is the interesting finding. The viral load was lower among the inpatients, that’s right, outpatients had higher viral loads. This inverse relationship held for the duration of symptoms to presentation. It was also true for the severity of illness – measured by the length of stay, the need for supplemental oxygen, and mortality. One of the implications of this is that the viral shedding, which common sense would suggest increases with viral load, would be much higher among the asymptomatic spreaders. (Another argument in favor of masks, if one was necessary). The findings also support a belief that once established, the disease course is not mediated by viral load so much as it is by our response. [1]
Here is the interesting finding. The viral load was lower among the inpatients, that’s right, outpatients had higher viral loads. This inverse relationship held for the duration of symptoms to presentation. It was also true for the severity of illness – measured by the length of stay, the need for supplemental oxygen, and mortality. One of the implications of this is that the viral shedding, which common sense would suggest increases with viral load, would be much higher among the asymptomatic spreaders. (Another argument in favor of masks, if one was necessary). The findings also support a belief that once established, the disease course is not mediated by viral load so much as it is by our response. [1]
Of course, every study has limitations, and the great weakness of the paper is that the quantity of virus was measured at only one point in time, so the actual viral loads over time are unknown. But this brings me to a second consideration, gleaned from an entirely different study on environmental factors in COVID-19. The cross-over between the two is based on mucus, what we all think of as a protective barrier – a physiologic sticky mat where the unlucky and unwary virus is trapped.
As it turns out, mucus is not inert “fly-paper,” but a biologically active secretion. Mucus contains mucins, glycosylated proteins – proteins with sugar attachments. These mucins, act as cellular decoys and cross-link with viral envelopes, found in COVID-19 among other viruses, binding them through an intermediary, a lectin, and subsequently inactivating the virus. The ability of mucus to act as a functional barrier has both an environmental and genetic component. From an environmental point of view, mucus needs to remain hydrated to maintain its structural qualities and viscosity or thickness. Decreasing its viscosity allows the cila of the bronchial tree to move them out of the lungs. Heating and air conditioning both remove humidity. As these authors suggest, “humidity on mucosal barrier may be a dominant molecular mechanism behind seasonality of respiratory viruses.”
Another fascinating cross-over fact is that many differences between humans in their microbial defense are “glycan-based.” If you find that term puzzling, ABO blood antigens are perhaps the best known among the general audience of you and me, of glycans. They are genetically derived, and the presence of an additional glycan, N-acetylgalactosamine, is felt to explain the greater susceptibility to COVID-19 for individuals with Type A blood.
Taking both of these studies together, what might we conclude or speculate. First, the quantitative measures used in the first study may well have captured COVID-19 particles that were present, but inactivated by mucus. So, while the test shows viral numbers, it fails to differentiate between active and inactive viruses. Viral cultures are difficult to grow, certainly more complicated, and time-consuming than bacterial cultures. Most of the testing for COVID-19 involves amplification of virus-specific DNA and RNA fragments which fail to distinguish between viable and non-viable virus.
Second, it adds another layer to our discussion of infectivity and susceptibility. Dysfunction of mucus or the ciliary activity necessary to move the mucus out of the respiratory tract, mucociliary dysfunction, is an overlooked defense and liability. Dry air reduces mucociliary function by increasing the viscosity of the mucus. That is something we can control with humidification systems and drinking lots of fluids. Parenthetically, I must mention that Alcohol is not among the beneficial fluids as it acts to net dehydrate you. [2] Mucociliary function is also affected by conditions outside our control, our genetic makeup. There is no “smoking gun” to explain COVID-19’s infectability; it is the mosaic of many factors. Some factors are quickly identified, like exposure and the response of our immune system. But other factors like mucociliary function are rarely considered, let alone measured. Among the many issues that the pandemic has surfaced is how truly little we know about why one person or another gets infected.
[1] Eastern philosophy would acknowledge that point of view quite readily believing we cannot control what happens to us, only our response to those events.
[2] Alcohol acts as a mild diuretic, increasing your urine output, which must be replaced to maintain hydration. It is this diuretic effect that is responsible for the saying that beer is never bought but only rented.
Sources: Association of Initial Viral Loads in SARS-cov-2 patients with Outcome and Symptoms American Journal of Pathology DOI: 10.1016/j.ajpath.2020.07.001
Effects of environmental factors on severity and mortality of COVID-19 MedRxiv preprint DOI: 10.1101/2020.07.11.20147157.




