Obesity is a description, not a “disease.”
Weight alone, by whatever measure, is only a marker for a more systemic problem, an unhealthy metabolism involving sugar and fat utilization. Weight is convenient because it is easily measured. Over time, the definition of obesity, excess weight that results in cardiovascular disease and diabetes, has changed. Weight was quickly replaced by Body Mass Index (BMI), which modified the weight by your height and gender. Then, like early phrenologists measuring various points on a skull, we have also identified waist circumference and waist-to-hip ratio as markers of unhealthy weight.
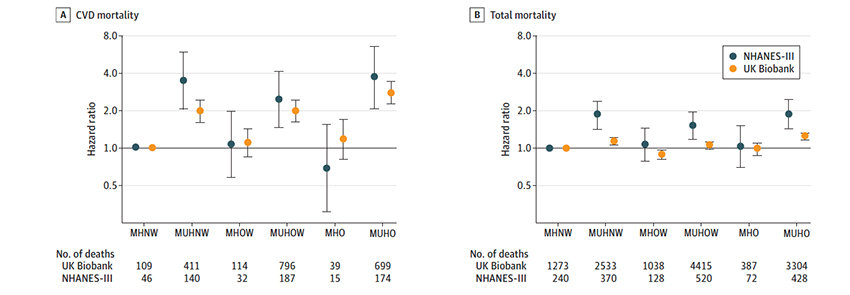
We thought we had the problem of excess weight solved until we found that some of those labeled obese had a healthy metabolism – one categorization became two, the metabolically healthy obese (MHO) and metabolically unhealthy obese (MUHO). A new article in JAMA Network Open tries to define what it means to be obese from the standpoint of cardiovascular risk. That is important because we focus energy on “obesity” to prevent cardiovascular disease and diabetes, so maybe some obese require more or less focus than others.
The Study
Researchers looked at individuals from the National Health and Nutrition Examination Survey (NHANES) between 1988 and 1994, and participants in the UK Biobank, a repository of genetic and health information. They used the information on weight and long-term health outcomes, specifically all-cause and cardiovascular mortality, to effectively separate the healthy and unhealthy obese. They used that information to determine the mortality risk of these participants based upon changing definitions of healthy obesity.
The dataset included about 12,300 NHANES participants of roughly equal genders and a BMI of 27 (“20% overweight”), followed for 14 years. The Biobank contributed 374,000, slightly more women, about ten years older, roughly the same BMI, and followed for 7½ years. NHANES contributed 1,758 deaths, 594 were cardiovascular; the Biobank had 12,950 deaths, 2,162 attributed to cardiovascular disease.
Time for statistical mathmagic
Previously, a healthy metabolism was characterized as:
- Waist circumference less than 40” for men, 34.5” for women
- Blood pressure (BP) of 130/85 without medication
- Triglycerides of 150mg/dL without medication
- HDL of >40 in men or >50 in women
- Fasting glucose of less than 110 without medication.
- Stricter criteria required a Hemoglobin A1c of <5.7 and total cholesterol of less than 240mg/dL without medication.
The authors did regression analysis to determine which factors seemed to have the most significant effect on mortality and found that they could more accurately define the metabolically healthy among the obese as those with
- Systolic BP 130 or less without medication
- A waist to hip ratio of 1.03 or less for men and 0.95 for women [1]
- No diabetes
Critically for the metabolically healthy obese, their mortality risk was no greater than that of a metabolically healthy, normal-weight individual – metabolic change, not weight per se, was crucial. These results were more robust in the American NHANES participants than the UK Biobank participants.
“BMI is considered an insufficient measure of body fat content because it fails to account for muscle mass and bone density and does not reflect fat distribution. Waist circumference is commonly used to capture abdominal obesity in prior MHO definitions; however, WHR is a more effective measurement of central adiposity, with WHR having the strongest gradient with incident CVD because not all excess weight is the same and will differ in its association with health risks.”
Ayana K. April-Sanders, PhD; Carlos J. Rodriguez, MD, MPH
Among the obese hoping to be considered metabolically healthy, an absence of hypertension was the most accessible criteria to meet. The absence of diabetes was the most difficult. 90% of each cohort’s obese had dysregulation of their glucose metabolism. The waist-hip ratio lay somewhere in between. But you had to have all three criteria, a situation true for 41% of the obese in the NHANES group and about 20% in the Biobank.
The Takeaway
While it is not surprising that the measurement criteria influence results, this study clarifies that weight per se is an inadequate means of determining your health or mortality risk. Weight and BMI are markers of possible underlying metabolic dysfunction; without a standard definition, unhealthy obesity remains enigmatic. What it does suggest, though, is that our emphasis on dysregulation of lipids, like cholesterol, while not misplaced, is overemphasized. Its inclusion did not enhance the ability to identify those at risk of dying from cardiovascular disease or any cause.
Excess weight can cause other medical issues. Significantly, it increases the trauma on our joints, so metabolically healthy obesity doesn’t mean your physician will not suggest some weight loss. But it seems that our healthcare energies and funding may better serve the “obese” if applied to preventing the onset of Type II diabetes. As I have written, I would hasten to add that identifying “pre-diabetes” to get a jump on the problem is no walk in the diagnostic or therapeutic park.
A bit of late-breaking news to throw more shade on obesity.
A report today in Lancet Diabetes and Endocrinology shows that the strong relationship between obesity, measured by BMI, and Type II diabetes noted in this study has a racial component. A study looking at 1.5 million general practice patients found that the incidence of Type II diabetes in Whites with a BMI of 30 was found at a BMI of 23.9 for South Asians and 28.2 for Blacks. Another wrinkle in a complex story [2]
[1] A waist-to-hip ratio of one means your abdomen is the same circumference as your hips. As you gain more fat added to your waistline, that ratio goes up. Fat added elsewhere doesn’t seem as critical.
[2] Ethnicity-specific BMI cutoffs for obesity based on type 2 diabetes risk in England: a population-based cohort study Lancet Diabetes and Endocrinology DOI: 10.1016/S2213-8587(21)00088-7
Source: An Empirically Derived Definition of Metabolically Healthy Obesity Based on Risk of Cardiovascular and Total Mortality JAMA Network Open DOI: 10.1001/jamanetworkopen.2021.8505




