Let’s begin with the data.
Infection or Severe Illness
The study involved those over age 60, high-risk populations, and health care workers who had received a 1st booster dose (3rd shot) at least four months previously and had not developed some degree of immunity (according to a prior PCR or rapid antigen) verified case of COVID-19. The Omicron variant was the predominant virus of concern.
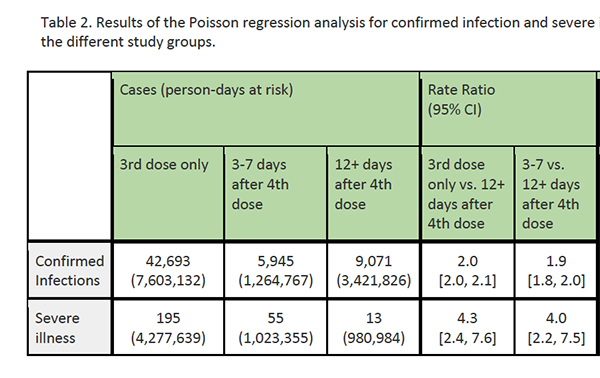
The study period included the first 12 days after the beginning of the vaccination program, chosen to stratify that population into those having received their second booster 12 days previously, 3 to 7 days previously, or not at all. The researchers felt that 3 to 7 days post-immunization was not sufficient to completely confirm additional immunity and would provide a second “control” group. Outcomes were the incidence of confirmed infections or severe illness [1] based on patient at-risk days. That denominator is a bit difficult to wrap one’s mind around easily but is simply the number of patients multiplied by how many days they were after the 2nd booster. [2]
Results
Those who did not receive the second booster were found to have twice as many confirmed infections and slightly more than 4-times more severe illnesses compared to people who did get the extra booster. The paper does not report any deaths in people who had either three or four shots. [The data show that the 2nd booster dose was more protective for these specific populations than the 1st given 4 months previously]. To generalize the target population, these results apply to any of us over 60 or at high risk [3]
Mortality
Mortality data concerning a 2nd booster comes from a second study involving members of one of the three large Israeli health organizations. Of the 563,465 eligible individuals, 58% received the 2nd booster. Co-morbidities among this population included hypertension, obesity, diabetes, and ischemic heart disease. Interestingly, only 6% had chronic lung disease, although 42% were current or prior smokers. Slightly more women opted for the 2nd dose, and “Uptake was notably higher in the older age groups and among participants with a higher socioeconomic status.”
There were 92 deaths among those receiving the 2nd booster vs. 232 among those having had only the first. The results were provided as hazard ratios where values below 1 were protective of the treatment group; in this case, those with a 2nd booster and values above 1 were at greater risk. The hazard ratio of a 2nd booster was 0.22 – it was significantly protective against death. Sub-group analysis by age is shown in the table. The second booster was protective from deaths in all age groups.
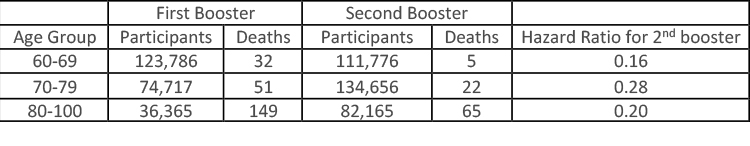 The difference between the second and third groups might reflect, in part, a survivor advantage – that among the very elderly, in addition to the frail, there are many resilient, “spry.”
The difference between the second and third groups might reflect, in part, a survivor advantage – that among the very elderly, in addition to the frail, there are many resilient, “spry.”
Safety
According to the FDA, their decision regarding the safety of a 2nd booster was based on the safety data previously gathered regarding Pfizer’s vaccine and a small study of 120 adults who received the 2nd booster of Moderna’s vaccine after a complete “course,” including the first booster, of Pfizer’s vaccine. No “new safety concerns were reported during up to three weeks of follow up after the second booster.”
What should you do?
Like all the doses that preceded it, the decision to get the 2nd booster should balance the risks and benefits. Those studies provide the best current information on the benefits. You must assess your risks. I am over 65 but have no other high-risk co-morbidities. But I am traveling to Europe in a month or so. I have a grandson, too young to vaccinate and, in reality, too young to become severely ill from COVID, but that doesn’t keep me from “worrying,” even if it is just a little. So, I will get the 2nd booster.
For those over 60 or immunocompromised, with one of those high-risk co-morbidities, the data demonstrate a benefit in terms of becoming ill or dying. “Long COVID” remains ill-defined, but one study indicates that more than 60% of those over 65 who experienced a COVID infection had one or more symptoms [4] of the long-form 90 to 180 days later. You do not get long COVID without having had COVID. Our experience of COVID is that it has a seasonal quality, tamping down in the summer, rising in the fall and winter. That might argue for waiting on that 2nd booster till later in the year when a new surge is anticipated. But how COVID behaves is not foreordained.
For the hesitant among us, uncertainty remains a plague upon our thinking. The Israeli data is short-term; you don’t precisely “match up” to the population studied; they had Pfizer’s vaccine you had Moderna’s. So many ambiguities. In this setting, consider more deeply your risk of becoming infected by COVID. You can begin with your lifestyle. Do you work in a public-facing job, take rapid transit? Just how exposed are you to others? And to what degree are those others transmitters of COVID; are enough people in your day-to-day world vaccinated to provide “herd immunity?”
We will decide whether to get that 2nd booster with the same calculus we have applied to the first and to being immunized – does our fear of becoming ill or dying from COVID outweigh our concerns about being vaccinated. It is the same calculus that had driven people to get their first or second booster before approval, stay home weeks before the government suggested it, or continue wearing masks when out and about. Do the risks of a 2nd booster outweigh your risk of getting COVID?
[1] Defined as “as a resting respiratory rate of more than 30 breaths per minute, an oxygen saturation of less than 94% while breathing ambient air, or a ratio of partial pressure of arterial oxygen to fraction of inspired oxygen of less than 300” – all markers of respiratory distress.
[2] 3 patients, two 12 days post-immunization, one 14 days post, would be 38 patient risk days.
[3] High-risk per the Israeli definition includes adults over age 65, residents of nursing homes and assisted living facilities, individuals on dialysis or with diabetes, cirrhosis, morbid obesity, or those immunosuppressed. It also includes those with acute heart conditions and exacerbation of chronic lung disease.
[4] chest/throat pain; abnormal breathing; abdominal symptoms; fatigue/malaise; anxiety/depression; pain; headache; cognitive dysfunction; and myalgia.
Source: Protection by 4th dose of BNT162b2 against Omicron in Israel medRx DOI:10.1101/2022.02.01.22270232
Second Booster Vaccine and Covid-19 Mortality in Adults 60 to 100 Years Old ORCID DOI: 10.21203/rs.3.rs-1478439/v1




