“I have not hitherto met with the record of any similar affection; and partly with a view of calling the attention of those practitioners who reside in the vicinity of the great coal mines, and who may have charge of the health of the miners, to the existence of a disease, to which that numerous class of the community would appear to be peculiarly exposed.”
George Pearson, an English physician, was the first to suggest that the darkening of lungs, seen during an autopsy, might be due to the soot inhaled from the burning candles, oil, and coal of 1813 life. Nineteen years later, a Scottish physician, James Gregory, connected those blackened lungs to coal miners and the coal dust they inhaled.
In the US, coal has been an energy source since the 1700s, especially in the area of “Pennsyltucky” – West Virginia, Kentucky, Pennsylvania, and a bit of Ohio. By 1920, coal fueled 70% of America; today, that percentage is roughly 18% - including 20% of the electricity that fuels those non-polluting electric vehicles. Black lung disease, coal workers’ pneumoconiosis, has been coal production’s fellow traveler.
 In 1968, a mine explosion was the catalyst among a coalition of disabled coal mine workers, the United Mine Workers of America, and the West Virginia Black Lung Association to bring an end to black lung disease. It took a strike involving over 40,000 miners to bring the coal industry in West Virginia to a halt and the legislature to the table to enact work protection. Within a year, the feds followed suit, including creating the Occupational Safety and Health Administration (OSHA).
In 1968, a mine explosion was the catalyst among a coalition of disabled coal mine workers, the United Mine Workers of America, and the West Virginia Black Lung Association to bring an end to black lung disease. It took a strike involving over 40,000 miners to bring the coal industry in West Virginia to a halt and the legislature to the table to enact work protection. Within a year, the feds followed suit, including creating the Occupational Safety and Health Administration (OSHA).
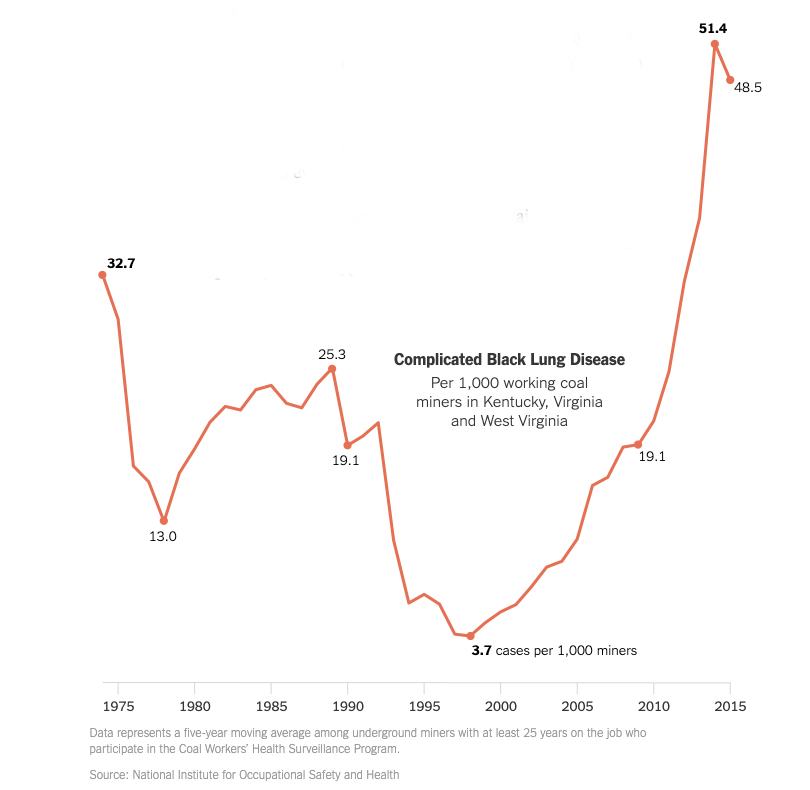
Black lung was dramatically reduced by regulations governing the amount of allowable coal dust in the mines and also by technological advances in how coal was mined and worker protection. But a little over a quarter-century ago, those gains reversed and the incidence of black-lung surpassed the carnage of years earlier, something that the New York Times graph shows. What changed?
Black Lung Disease
Black lung disease is medically classified as a pneumoconiosis, a disease within the lung tissue causing inflammation followed by scarring, and fibrosis. The fibrosis slowly but surely reduces the ability of the lungs to expand and take in air as well as the lung’s ability to transfer oxygen into the bloodstream. It is the same pathological process seen in those TV ads by lawyers on the hunt for cases of asbestosis. It is also caused by silica, a mineral we will see again in our tale. Coal worker’s pneumoconiosis (CWP), another name for black lung disease, exists along a spectrum with a more virulent form, progressive massive fibrosis (PMF). There is no cure and, to be fair, no satisfactory treatment – all we can offer is oxygen or, perhaps, a lung transplant.
It takes 10 years or more for the cumulative effects of coal dust to begin to become symptomatic and apparent. CWP is a quiet thief, stealing your ability to engage in life; it can be profoundly disabling. Just imagine if your world consisted of only a portion of your home, even then, tethered to an oxygen line.
The Federal Coal Mine Health and Safety Act of 1969
“…an incurable disease caused by inhalation of coal dust…it is not caused by smoking” and “…is easy to distinguish with x-rays.”
- Dr. David Blackley, head of Respiratory Disease Studies, National Institute for Occupational Safety and Health
In addition to setting standards for dust levels, this legislation created the Black Lung Disability Trust, funded by a federal coal tax. Two clauses in that legislation are pertinent today:
- Miners with a 10-year history of mine work and X-ray evidence of severe lung damage [1] are guaranteed compensation.
- Miners have “rate retention,” allowing them to transfer to jobs with lesser amounts of dust exposure while maintaining their pay, seniority, and benefits
Why the increase?
“The government can claim they are doing all they can to reduce miners’ exposure to coal mine dust and operators can argue the industry isn’t at fault, but there is clearly a problem here. There is only one way miners get Black Lung disease. They are breathing air that contains excessive amounts of respirable coal dust. Having stated the obvious, it becomes clear that the law is not being properly enforced or mine operators are not following mandatory health and safety standards or both. There is no other explanation.”
- Cecil Roberts, President of the UMWA
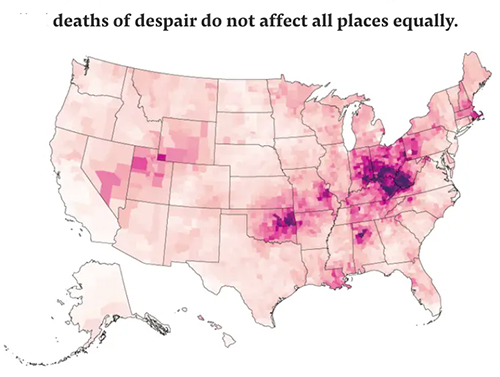 Mr. Roberts is only partially correct. It is always more complex, and it begins with improvements in mining machinery that increased the efficiency of coal mining operations – another way of stating that it required fewer miners to produce the same amount of coal. That increased productivity brought a great deal of unemployment, economic hardship, and despair to coal country. It is no coincidence where those “deaths of despair” from overdoses and alcoholism, and suicide reside. Mining jobs were some of the best paying, albeit dangerous, jobs in the area – so having one of the few remaining jobs in the mines became even more precious.
Mr. Roberts is only partially correct. It is always more complex, and it begins with improvements in mining machinery that increased the efficiency of coal mining operations – another way of stating that it required fewer miners to produce the same amount of coal. That increased productivity brought a great deal of unemployment, economic hardship, and despair to coal country. It is no coincidence where those “deaths of despair” from overdoses and alcoholism, and suicide reside. Mining jobs were some of the best paying, albeit dangerous, jobs in the area – so having one of the few remaining jobs in the mines became even more precious.
The efficiency of mining machinery also led to rapidly dwindling sources of easily mined coal despite a persistent demand for the fuel. To get at more coal, the miners simply had to dig deeper through rock that contained the seams of coal. The rock also held a great deal of silica, and silica creates far more inflammation and fibrosis than coal dust alone. In fact, it is probably the smaller amounts of silica in easily mined coal that was responsible for CWP all along.
Rising Levels of Silica
A new study in the Annals of the American Thoracic Society demonstrates the rising levels of silica in the lungs of coal miners. The researchers compared lung tissue taken from miners born between 1910 and 1930 (those working before modern mining technology) and those born after 1930 – the more contemporary miners. They looked at the characteristic nodules that form in CWP, categorizing them on silica content. The “historic” miners had a higher percentage of nodules predominantly with coal dust, 50% - threefold more than contemporary miners. The current miners had a higher percentage of nodules predominated by silica, 57%, three-fold more than historical workers. The reason for the greater amounts of silica, a known carcinogen, was all that granite they now had to dig through to get to deeper layers of coal.
“These findings provide the first direct evidence that silica is a causative agent behind the increasing incidence of progressive massive fibrosis — severe black lung disease. This is critical information that can be used to determine health-protective permissible exposure limits for coal miners,”
– Robert Cohen, MD, lead author, Respiratory Health Division, National Institute for Occupational Safety and Health
In 2019, the Mine Safety and Health Administration, the OSHA equivalent specifically for mine safety and health, requested information to change the regulations regarding silica. The Office of the Inspector General issued a report in 2020 concluding that the silica regulations were out of date, sampling was too infrequent to “be sufficiently protective,” and that no fines could be levied because silica levels were tied to coal dust exposure limits. Two years later, there has been no action on the recommendations to reduce exposure to a known carcinogen, increase sampling, and establish a separate standard for silica. The current standard is 100 micrograms/cm3, but most of us, with no exposure to silica, need not worry; OSHA’s standard for our workplaces is 50 micrograms/cm3 – only those miners at high-risk operate under laxer standards.
The Low Participation Rates of Screening
 Why, as this graph shows, are fewer miners being tested despite a rising tide of illness? A study looking at this issue found that of the 18,000 underground miners in West Virginia in 2015, only 1200, 6.5%, had been tested; 16% of these were positive. The authors identified several issues.
Why, as this graph shows, are fewer miners being tested despite a rising tide of illness? A study looking at this issue found that of the 18,000 underground miners in West Virginia in 2015, only 1200, 6.5%, had been tested; 16% of these were positive. The authors identified several issues.
- Testing is often logistically difficult – Diagnostic centers are often placed an hour or more drive away from the mines, and there is no paid “time-off” to get tested.
- There are disincentives – State legislation places one or two-year statutes of limitations on compensation claims. Once you are diagnosed, the clock on obtaining workers’ compensation is running; your mining job, the most lucrative job where you live, will end in 4 to 5 years. Remember the right to ask for a job with less dust exposure? It does exist but comes with some social stigma and fear, rationale or not, of economic retribution. It is a rarely exercised “right.” When exercised, it is often near the end of a mining career, long after the harmful effects of coal dust and now increasing amounts of silica have initiated your respiratory decline.
- Work and family are entwined. Miners often go back generations, and mining, despite all of its dangers, still represents the means to successfully support your family. Miners’ self-esteem is, in part, predicated upon the difficulty and hazards of their work. Even with no economic loss, taking on a lesser role comes at a psychic price.
I had thought that Black Lung Disease was in our past. As is often the case, I was late in getting the memo. For various reasons, technology, economics, and human behavior Black Lung Disease is alive and well. Changing the regulations to protect these American citizens should be as much and as important a priority as moving away from coal as a fuel source.
[1] The pattern of changes from CWP on an X-ray of the chest is diagnostic of the condition in coal miners and does not require a tissue biopsy.
Sources: Pathology and mineralogy demonstrate respirable crystalline silica is a major cause of severe pneumoconiosis in US coal miners Annals of American Thoracic Society DOI: 10.1513/AnnalsATS.202109-1064OC
The enduring legacy of black lung: environmental health and contested illness in Appalachia Sociology of Health and Illness DOI: 10.1111/1467-9566.12777
The real story about miners, Black Lung and the life and death struggle for benefits United Mine Workers of America
The Militant Miners Who Exposed the Horrors of Black Lung JSTOR Daily




