How are politicians similar to bacteria? ACSH advisor Dr. Henry Miller explains.

As an undergraduate and grad student, I cut my research teeth working on bacteria. I found their resilience to be amazing; they’ll do anything to survive. If you cultivate them in growth medium with modest amounts of an antibiotic and examine the genetics of the ones that aren't killed, you find mutations of various kinds. For example, some will cause the bacterial cell wall to become impermeable to the drug, or that make the intracellular target resistant to it, or that rapidly metabolize and get rid of the drug. And radical genetic changes enable bacteria called extremophiles to adapt to hostile environments, such as in conditions of extreme temperature, acidity, alkalinity, high pressure, or the absence of oxygen.
Politicians are similar to bacteria. They adapt to changing circumstances. Although many are committed to their principles and consistent, at least as many pander, reverse positions, make promises they have no intention of keeping, and sometimes implement policies that their constituents want but that are unwise or even injurious. Welcome to the COVID-19 pandemic.
A cynical example of sacrificing the protection of public health to political expediency is the Biden administration’s abandonment of sound scientific responses to the still-persisting pandemic. As revealed in investigative reporting by Rachel Levy of Politico, in recent months administration officials privately discussed how many daily COVID-19 deaths would be acceptable to the public in order "to declare the virus tamed." According to Levy:
One of the three people involved in the conversations last year said it was an effort to gauge what the American public would "tolerate."
"Five hundred [deaths] a day is a lot. You still have 9/11 numbers in a week," the person said. "People generally felt like 100 [a day] or less, or maybe 200, would be OK."
With fewer than 200 people dead per day, the person added, hospitals wouldn't be overrun and infection rates would be comparatively low, allowing Americans to live closer to pre-pandemic times with less threat of infection.
"When you spread 100 to 200 [deaths] around the country, then it's minimal around your [geographic] area," the person said.
In the end, the administration political operatives seem to have settled on a higher number. A much higher number: On July 29, the deaths were 618 and the 7-day average was 432. COVID-19 hospitalizations were also trending upwards, especially in people over 70 years of age. But in spite of those worsening COVID numbers caused by the highly transmissible Omicron BA.5 subvariant, except for updates about President Biden’s COVID-19 infection, federal officials have been largely Missing in Action for weeks.
Are we at a new peak for this variant? According to the CDC, as of July 29, “most of the country is reporting moderate to high SARS-CoV-2 levels in wastewater. Around 53% of sites are currently seeing some of the highest levels for those sites since December 1, 2021.” That’s not an encouraging sign in a useful early indicator.
The number of U.S. cases of COVID-19 is difficult to estimate because most people are testing at home or not testing at all. As of the end of July, the official, confirmed number of cases/day was around 130,000 but infectious disease experts say that that wildly underestimates the true number by several fold.
These statistics indicate a dire complication of COVID infection: long COVID, or "post-COVID conditions," the persistence for weeks, months, or years of post-infection symptoms that can affect many organs and be extremely debilitating. The numbers are difficult to pin down, because of inconsistencies in definition and reporting, but here is the CDC's most recent statement:
Estimates of the proportion of people who had COVID-19 that go on to experience post-COVID conditions can vary:
- 13.3% at one month or longer after infection
- 2.5% at three months or longer, based on self-reporting
- More than 30% at 6 months among patients who were hospitalized
Thus, we could be seeing tens of thousands of new cases of long COVID every day, which would be catastrophic, not only for individuals but also, long-term, for businesses (because of absenteeism) and our healthcare system.
A physician who is a senior executive for one of the nation's largest healthcare insurers told me that they are seeing claims for COVID-infected patients who need long-term support on ECMO (extracorporeal membrane oxygenation), an apparatus similar to an operating room heart-lung machine, whose hospital bills run into the tens of millions of dollars.
The inescapable conclusion is that we need to redouble our efforts to prevent COVID infections, not decide arbitrarily on metrics to pretend that the threat of the pandemic is over and it's time to "move on."
The measures should include:
- Mask and vaccine mandates (including boosters) for airports, flights, public transportation, and indoor public events at which large numbers of people are congregating
- Realistic, science-based quarantine and isolation recommendations — five days isolation after onset of symptoms is not sufficient for many patients
- The CDC's definition of "fully vaccinated" should include two boosters for everyone over the age of five years
- An aggressive public-private effort to improve ventilation in buildings
- Frequent, strategic testing (e.g., before boarding planes or cruise ships or attending events at which crowds will congregate indoors)
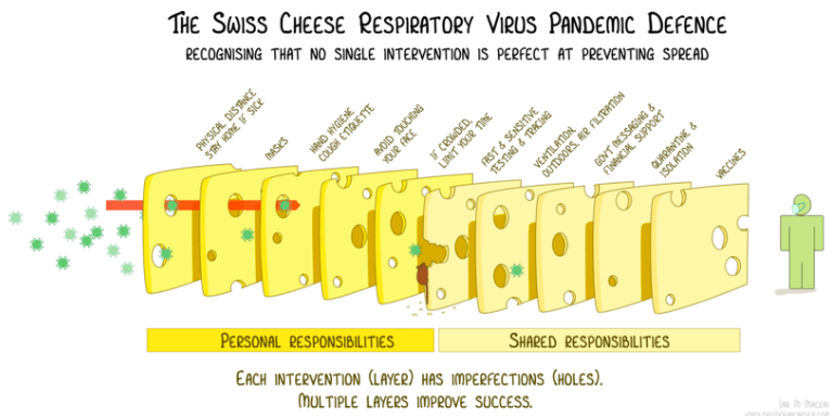
- Public Service Announcements by public health officials, politicians, and celebrities, all emphasizing the importance of the "Swiss Cheese Model of Prevention," a graphic illustration of what can and should be done recognizing that no single intervention is sufficient to preventing spreading infections (below)
As George Washington University medical school Professor of Medicine and Surgery Jonathan Reiner tweeted on July 16th: “97% of the US now has high or substantial transmission. I doubt there's ever been this much COVID blanketing the entire country during the pandemic. Still no push for any mitigation. This is what capitulation looks like.”
(And keep in mind that every infection involves more virus replication, more mutants, and the opportunity for Darwinian evolution to select for new, more "fit" and more worrisome variants of concern.)
Dr. Lucky Tran, science communicator at Columbia University Medical Center, was more pointed, tweeting to CDC Director Rochelle Walensky on July 14th: “If you are serious about preventing more death and disability, why are you not pushing for a comprehensive layered public health strategy that includes strong mask policies?”
The answer seems to be that Walensky, White House COVID coordinator Ashish Jha and their political bosses have taken the pulse of the public and they’ve decided not to act even though the data indicate the need for quick and decisive intervention. A recent New York Times poll of registered voters found that fewer than one percent placed the pandemic as their top priority.
In the face of widespread pandemic fatigue, it seems that Walensky, Jha, and presidential advisor Dr. Anthony Fauci, who surely know better, have decided not to impose unpopular restrictions or deliver bad news to the public in an election year, but merely to occasionally deliver tepid, non-binding recommendations.
That is a cynical course of (in)action. Bitter medicine is needed to keep a bad situation from becoming even worse. But, hoping that it will help them survive politically, the bacteria-like politicians have other ideas.
Henry I. Miller is a physician and molecular biologist. He was a Research Associate at the NIH, the founding director of the FDA's Office of Biotechnology, and a consulting professor at Stanford University's Institute for International Studies. Find Henry on Twitter @HenryIMiller
Note: This is an updated and revised version of an article published by the Genetic Literacy Project.
