Increasing concerns about long-haul COVID (LHC) have appeared in the popular press but less frequently in the medical literature. The PubMed database lists 32,922 review papers on COVID-19 but only 196 on LHC. Underlying these statistics is the realization that there are no objective diagnostic criteria, tests, or biomarkers – LHC is a “diagnosis of exclusion,” and its pathophysiology remains unknown.
What is long-haul COVID (LHC)?
A recent summary of LHC quoted a White House memo that defined three groups of persons who may have experienced LHC: those with lingering physiological conditions, behavior changes, and those grieving loss of loved ones. Here, we focus on the first group, those with signs and symptoms.
- Fatigue (58%).
- Shortness of breath (21%).
- Pain (19%).
- Cough (19%).
- Memory loss (16%).
Daily COVID-19 outcomes aggregated to counties, states, and the nation have been based on official medical records such as hospitalizations, deaths, and vaccine doses administered. Still, data on LHC patients‘ age, education, or income are not included. We have supplemented our daily analyses with data from the U.S. census, assuming that census tract or state averages apply to individual residents. Possible errors in reported COVID outcomes include undercounting or misdiagnosis; we view the data as rigorous but not specific.
LHC is not a recognized disease per se but is defined by the timing of various symptoms occurring after a previous diagnosis of acute COVID. LHC data are based on public surveys and represent individual opinions rather than medical diagnoses. Sources of error include lapses in memory, overemphasis on symptom duration, psychosomatics factors, and varying definitions. These surveys include data on individual characteristics unavailable from the CDC; we regard LHC data as specific but not very rigorous.
Our analysis is strictly “number crunching” with no medical implications. We are simply trying to interpret public data labeled as LHC, however defined.
The Household Pulse survey is a 20-minute online survey “designed to deploy quickly and efficiently and to collect data on household experiences during the coronavirus pandemic.” The results are then scaled to reflect the entire nation and are broken down by specific characteristics. For LHC, respondents reported:
- 20.7% currently have symptoms.
- 30.4% had symptoms for more than three months.
- 82% had received a COVID vaccine.
- 33% had or planned to receive a COVID booster.
- 7.6% (25 million) currently experience LHC; 14.8% (49 million) have ever experienced it. We believe this may be an undercount.
Here are the LHC national survey results stratified by educational level, racial grouping, and age group.
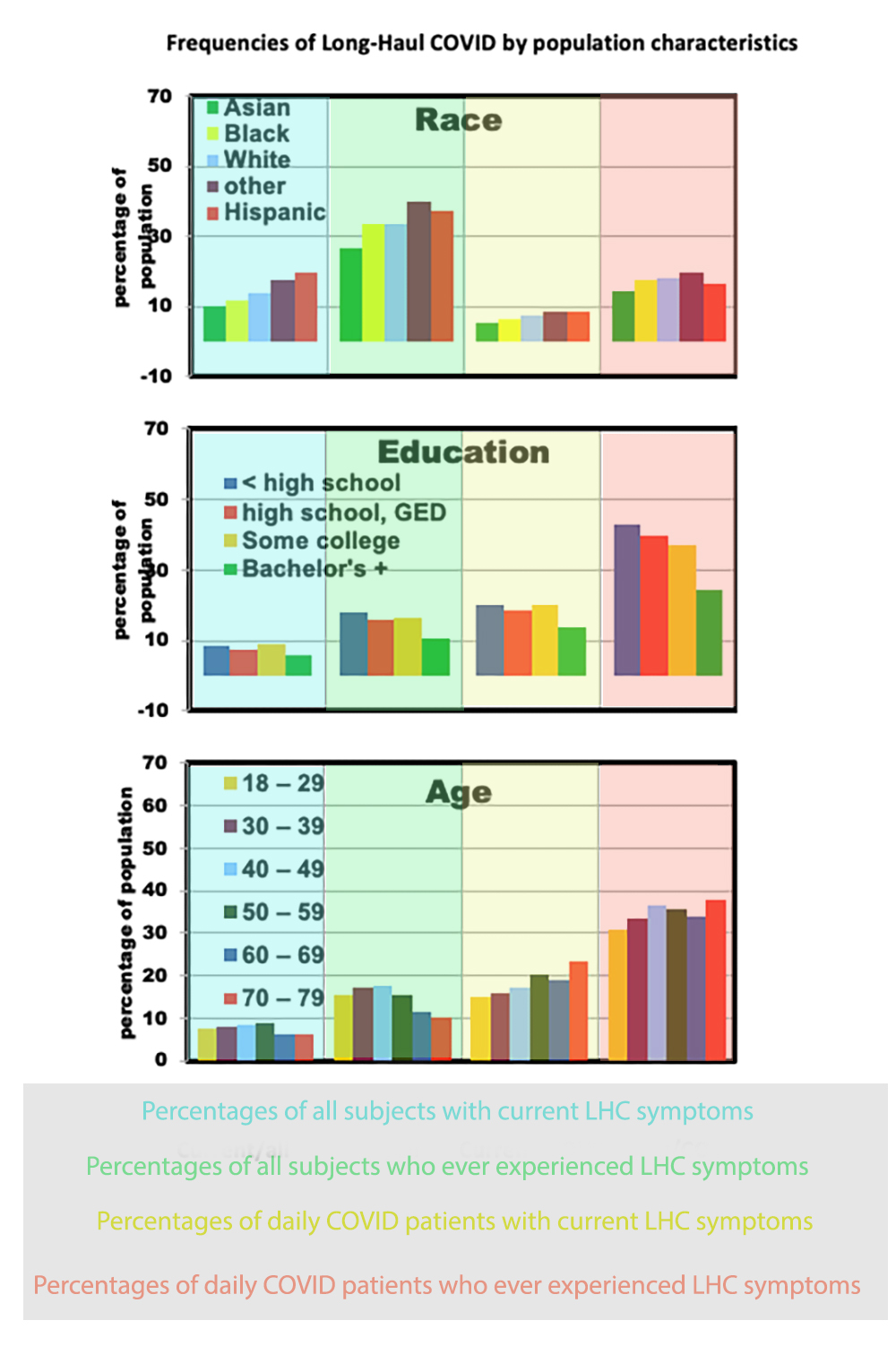
The three graphs show that:
- Young and middle-aged adults had higher LHC risks among all adults but not as percentages of COVID cases.
- This was also the case for Hispanics; Asians had the lowest risks.
- Higher education was uniformly beneficial in reducing LHC symptoms.
We compared the stratified groups by their respective vaccination rates for initial and booster vaccination and the presence of acute COVID or ever having symptoms lasting three months or more.
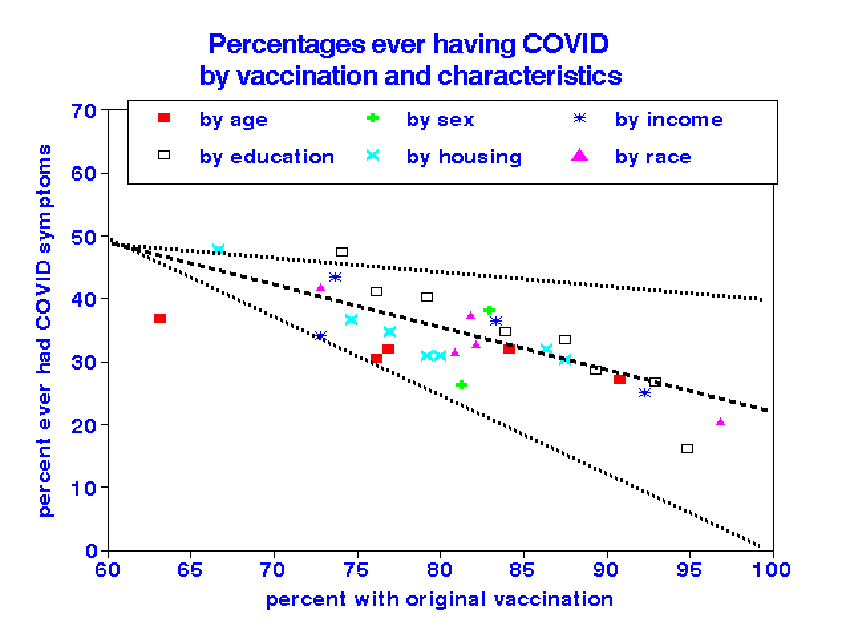
When the Household Pulse Survey population is stratified into six groups by demographics, vaccination status is the most critical determinant of LHC symptoms - within-group differences in LHC was likely due to differences in their vaccination rates than demographics.
About 25% of the cumulative daily cases were associated with total vaccinations, compared with 32% of LHC cases, indicating an equivalent role.
In December 2020, the CDC initiated the Inspire Trial, a prospective longitudinal cohort study of adults comparing self-reported symptom prevalence between those who tested positive or negative for COVID-19. Volunteers were solicited from the metropolitan areas of Seattle, Los Angeles, San Francisco, Houston, Dallas, Connecticut, and Philadelphia. However, the cohort is not demographically representative of the US, comprising:
- 66% males
- 57% aged 15-40, 34% ages 41-64
- 71% with at least some college
- 65% White, 12% Asian.
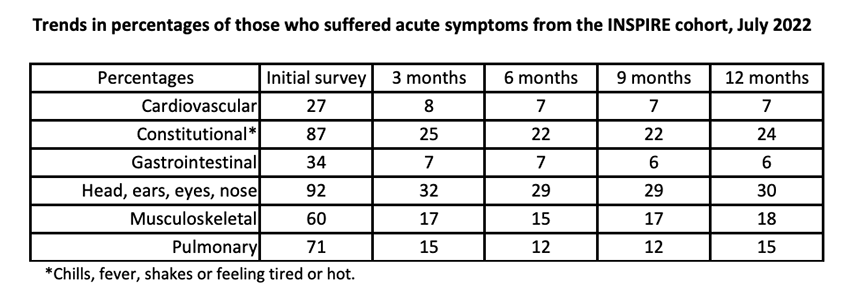
The data on 4113 INSPIRE patients show 35% with prolonged symptoms but essentially no further symptomatic changes 3 months after acute infection. Respiratory and “constitutional” symptoms are the most common. However, the study is much too small to yield information on effects of personal characteristics on LHC; only 23 participants reported cardiovascular symptoms at 12 months, and only 51 reported pulmonary symptoms. This is a typical epidemiology Hobson’s choice: either too few subjects or less information about each of them.
Parting Thoughts
There is no consistent clinical definition of long-haul COVID and comparing various survey results depends on their demographics. Differences in vaccination coverage may account for most of the diversity. Our findings must be tempered by likely uncertainties in the validity of self-reported symptoms. Despite ambiguity in definitions, our analyses achieved highly statistically significant associations but did not address clinical findings. The INSPIRE study is intended to include medical records but neglects vaccination status and is too small to yield useful results. Existing studies of LHC are unlikely to identify any important individual characteristics leading to LHC beyond vaccination status.
“Long-haul COVID-19 deserves much more attention”
Sources: Perspective. Confronting Our Next National Health Disaster – Long-Haul Covid. NEJM DOI:10.1056/NEJMp2109285



