“All things are poisons, for there is nothing without poisonous qualities. It is only the dose which makes a thing poison.”
―
Starting in 1993 and extending for more than a decade, the Journal of the American Medical Association (JAMA) began publishing a long series of “users guides” and other publications that championed the emerging trend toward clinical epidemiology and evidence-based medicine (EBM), in which a tight focus on “high level” evidence was paramount. JAMA Internal Medicine appears to have strayed far from its own EBM principles, in now publishing an article entitled “Projected Lifetime Cancer Risks From Current Computed Tomography Imaging”, asserting that CT scans will cause one million excess cases of cancer in the coming decade. In the article, the authors write that
“To empirically quantify lifetime risk would require decades-long follow-up studies of very large populations.”
The authors thereby acknowledge to editors and readers that they offer no empirical evidence that radiation from computerized tomographic scans performed for screening and diagnosis has caused cancers in adults, and that such evidence is unlikely to be forthcoming in the foreseeable future.
While EBM demands empirical evidence before diagnostic or therapeutic interventions are accepted into clinical practice guidelines, this article fails to cite any empirical evidence of low-dose radiation carcinogenesis in adults, offering only modeling based upon the controversial linear, non-threshold theory. Moreover, the estimated frequency of excess cancers has accelerated alarmingly since the author, Dr. Smith-Bindman’s initial 2009 prediction that CT scans would cause 29,000 cancers. Today, the incidence of excess cancers caused by CT scans has somehow risen from 2% in 2009 to 5% in 2025 - a puzzling surge amidst concerted efforts to reduce CT radiation exposure throughout the U.S..
In my previous article, I briefly discussed the controversy surrounding the linear, no-threshold theory of radiation carcinogenesis, which Dr. Smith-Bindman relied upon in her modeling projections. A brief reconsideration here appears appropriate. The first principle of toxicology is the dose-response relationship. Even deadly poisons can have a limited or even beneficial effect at low dosage. Botulinum toxin is among 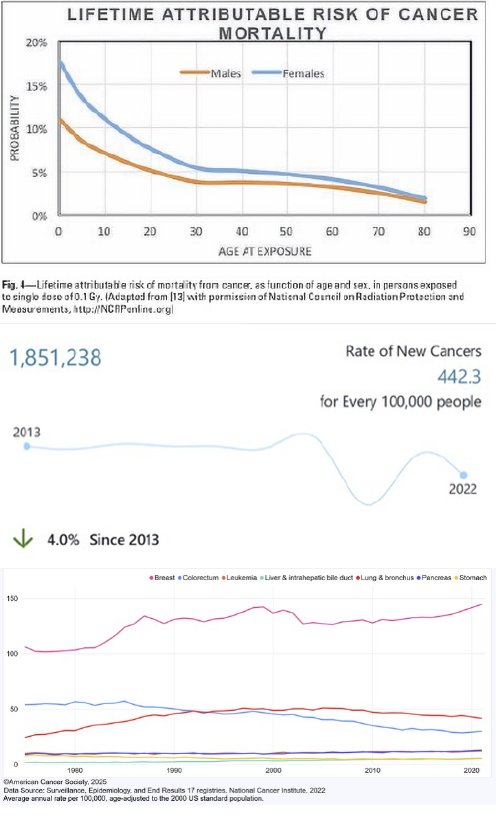 the most toxic substances, with an LD50 of 1 nanogram per kilogram, i.e., 70 billionths of a gram will kill 50% of those exposed. Despite such astonishing toxicity, commercial pharmacological sales of “Botox” exceed five billion dollars annually. The comparable LD50 for ionizing radiation is 3-5 Gy, equivalent to approximately 3,000-5,000 low-dose chest CT scans.
the most toxic substances, with an LD50 of 1 nanogram per kilogram, i.e., 70 billionths of a gram will kill 50% of those exposed. Despite such astonishing toxicity, commercial pharmacological sales of “Botox” exceed five billion dollars annually. The comparable LD50 for ionizing radiation is 3-5 Gy, equivalent to approximately 3,000-5,000 low-dose chest CT scans.
There remains no question that there is powerful evidence that high doses of radiation can cause cancer, typically after an interim delay of many years. There is also evidence, primarily based upon risk of cancer in survivors of atomic bomb explosions, that a dosage as low as 0.1 Gy may increase the risk of subsequent cancer. Risk is primarily dependent upon radiation dosage, but age and gender at the time of exposure are also important factors.
To date, the only data suggesting a risk of cancer at doses lower than 100 mSv, from diagnostic radiation exposure, relate to increased risk of leukemia and brain tumors in children after CT scans. While CT scans have markedly increased over the past two decades, cancer rates have gone steadily downward - the age-adjusted incidence of cancer, 466.8 per 100,000 in 1975, and then fell slightly to 443 in 2022
There is, accordingly, no empirical evidence from cancer registries suggesting an increase in new cancers; rather, incidence has declined.
What about specific organ cancers? Dr. Smith-Bindman estimates that CT scans will cause 21,400 new lung cancers, 8400 colon cancers, and 7400 leukemias. Annual incidence data shows that both lung cancer and colon cancer incidence and deaths have fallen sharply, and leukemia incidence has risen slightly from 10/100,00 to 12/100,000 between 2000 and the present.
There is a second problem with the article that requires consideration. In Dr. Smith-Bindman’s conflict of interest statement, she reports that, “this work does not overlap with Alara’s commercial activities.”
What exactly are Alara’s commercial activities? In 2019, CMS invited researchers and experts to develop a measure for CT scans, utilizing financial incentives to enhance clinical outcomes and safety. Alara Imaging, founded by the author and her husband, provides “free” services to enable providers to transmit compliance data to CMS, thereby qualifying for payment advantages. “Free” is somewhat misleading, as the Alara website explains that while their basic service is free, to “access more powerful features,” you need to “pay as you go.”
Hyperbolic cancerphobia, generated by media reports on this study, may serve to drive up sales of Alara services. This is a clear financial conflict of interest. Far more concerning, if the content of this article is accepted as accurate, it might be expected to unreasonably deter adults from accepting a beneficial diagnostic test with adverse consequences.
As Mark Twain observed, “Common sense is not that common”. It would defy common sense to accept an allegation, unsupported by empirical data, that low-dose radiation from diagnostic CT scans in older adults will cause large numbers of cancers within a short latency period. It just doesn’t make sense.
When predictive models outpace empirical reality, we risk replacing science with sensationalism. The assertion that CT scans are fueling a cancer surge in adults isn’t supported by real-world evidence and may do more harm than good by deterring lifesaving diagnostics. Let’s not allow poorly grounded fear, academic self-interest, or profit motives to obscure what matters most: patient outcomes grounded in common sense and actual data.
Note:The author has a potential conflict of interest, as he has been an IELCAP investigator since 2001 and has received reimbursement for travel and accommodations for participation in semi-annual research meetings. He has provided paid expert witness testimony in three class action medical monitoring lawsuits against Philip Morris.
Additional Sources: Radiation Risk to the Fluoroscopy Operator and Staff American Journal of Roentgenology DOI: 10.2214/AJR.16.16555


