“All models are wrong, some models are useful.”
Those are the words of George Box, considered one of the brightest of our 20th-century statisticians. With those words in mind, this paper's researchers developed a COVID-19 pandemic model that incorporated our behavioral response, e.g., masks, social distancing, economic lockdowns. The goal was not so much to predict the outcomes of lives or money lost; it was to try and describe how those trade-offs altered the path to reach the pandemic’s end (or not).
They found that tiny changes in the underlying assumptions, compounded by our changing responses to the virus, resulted in complex behavior:
“with secondary waves and surges with accompanied business and school re-closures and shutdowns [making] accurate projections under such circumstances unlikely.”
The basic pandemic model, the Susceptible, Infected, Recovered model, follows the virus's evolving behavior but treats the hosts, that would be us, as unresponsive, only becoming infected, dying, or recovering - making no attempt to avoid viral infection. The researchers added our behavior, the social distancing, and the closure of commerce into the equations to see how the outcomes and trajectories changed.
"The key to the formulation of this model mathematically is the insight that optimizing behavior under conflicting health and economic incentives can drastically change epidemic dynamics and outcomes."
Ronan Arthur, postdoctoral research fellow, Stanford University School of Medicine
The greater the number of infections, the more we adhered to preventative measures, creating a negative feedback loop on the incidence of viral infections. By itself, that complicates the model because now there is a dance between the virus and host. The dance, really the path to an outcome, is further complicated because our behavior lags behind that of the virus; there are delays in recognition, testing, reporting. And variations in how our behavior changes once these signals are recognized and considered.
Remember last spring when COVID-19 was a problem confined mostly to the urban Northeast? This was before it began to fill in the heartland and rural areas. Or how seniors in Florida started staying home long before any declaration from the Governor while youth continued to party? It was both our adherence to preventative measures and our delays in implementing them that the researchers sought to model.
They incorporated a variable, technically called a “utility function,” that optimized the number of social contacts the susceptible and infected hosts might have based upon “perceived risks and benefits of social contacts.” The variable allowed individuals a trade-off between infection and social contacts and for governments to trade-off increasing infections with the need to restore the economy.
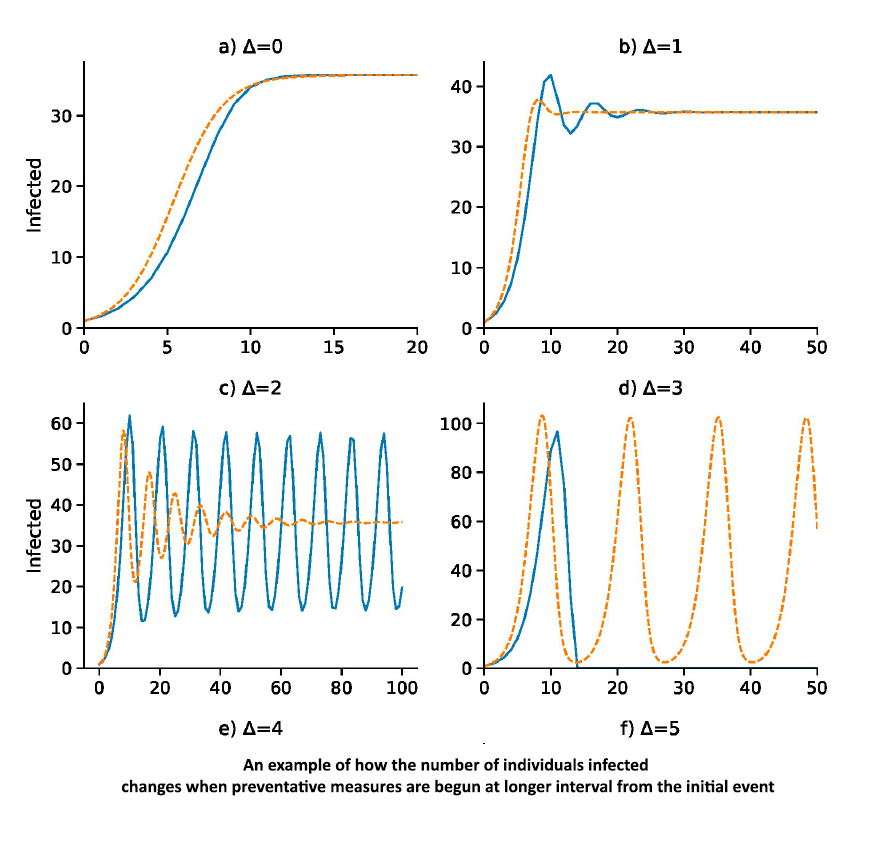 They found that small changes in the trade-offs compounded by delays in acting upon those decisions resulted in more than one possible outcome. In some cases, the epidemic came to an end; in others, it reached what we might consider herd immunity with a small number of people sacrificed to the virus but the majority protected. But these were not the only outcomes, as the graph to the left demonstrates. Some alterations resulted in a secondary surge of infections or in a dampening wave of more and fewer cases over time. Their model varied our behavior, not the virus’s behavior in terms of infectiousness or lethality. Demographics, host immunity, seasonality, and “socio-cultural idiosyncrasies,” all parts of our common media’s narrative of causes, do not necessarily explain the ups and downs of COVID’s caseloads.
They found that small changes in the trade-offs compounded by delays in acting upon those decisions resulted in more than one possible outcome. In some cases, the epidemic came to an end; in others, it reached what we might consider herd immunity with a small number of people sacrificed to the virus but the majority protected. But these were not the only outcomes, as the graph to the left demonstrates. Some alterations resulted in a secondary surge of infections or in a dampening wave of more and fewer cases over time. Their model varied our behavior, not the virus’s behavior in terms of infectiousness or lethality. Demographics, host immunity, seasonality, and “socio-cultural idiosyncrasies,” all parts of our common media’s narrative of causes, do not necessarily explain the ups and downs of COVID’s caseloads.
The researchers did not offer a prediction of how the pandemic might end, nor do they opine on what individuals or the government should be doing or be doing differently. They end with this concern.
“Lags, whether social, environmental, or biological, mean that people can respond inappropriately to an unfolding epidemic crisis, but they also mean that people can abandon protective behaviors prematurely as conditions improve.”
Just as being vaccinated is not a license to no longer wear a mask, social distance or wash your hands, the decreasing rates of COVID-19 infections are not a clear signal that the lockdowns “worked,” and we can immediately return society to normal. We should be aware that as we inch closer to herd immunity from the combination of vaccinations and those who have recovered, there will be less and less incentive for the hesitant to be vaccinated; after all, it is always someone else’s responsibility, not theirs.
Source: Adaptive social contact rates induce complex dynamics during epidemics PLOS Computational Biology DOI: 10.1371/journal.pcbi.1008639




