Let’s get right to it. The data on the top 22 high-income countries comes from the Organisation for Economic Co-operation and Development (OECD), specifically estimates of expenditures on cancer care for 2019. The Globocan database, a registry maintained by IARC, provided the “age-standardized cancer mortality rate estimates in 2020 for the 22 selected countries, including all 36 cancers represented in the database.”
Here are the basic findings. I have removed some of the columns to provide a bit more focus.

- Median cancer mortality was roughly 70 deaths per 100,000 population
- Cancer mortality, with or without consideration of smoking, did not correlate with cancer care spending. There was also no difference when accounting for the purchasing power of consumers in each country. [1]
- While we spent the most on cancer care, nine countries spent less and had fewer deaths.
- Compared to countries with higher mortalities, we spent more, by at least $1 million to avoid additional deaths; in some cases, as much as $5 million more.
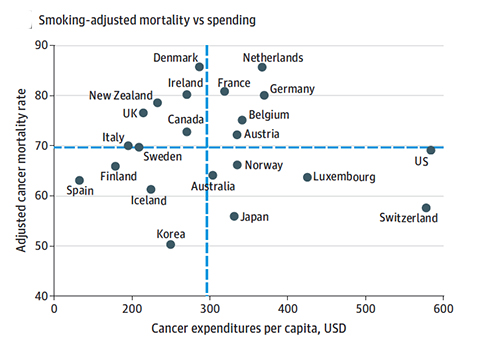 This table captures those bullet points. In short, when it comes to cancer mortality, we are not getting as much “bang for our buck” as many other countries. Simply spending money does not result in fewer deaths. As the authors write,
This table captures those bullet points. In short, when it comes to cancer mortality, we are not getting as much “bang for our buck” as many other countries. Simply spending money does not result in fewer deaths. As the authors write,
"Compared with the remaining countries with higher cancer mortality rates, the US additionally spent more than $1 million per averted cancer death."
The authors offer some explanation for our greater costs. Of course, we must begin with the cost of drugs; US drug prices subsidize the costs for the rest of the world; we may pay more, so other countries pay less. Additionally, unlike the UK’s National Institute for Health and Care Excellence (NICE), the FDA does not approve drugs based on efficacy and cost, so some new and more expensive drugs "often confer marginal or unclear survival gains.” There are also costs to some of our care guidelines, we are often more aggressive in screening for disease, in treating disease that might well be observed, and we frequently spend more on end-of-life care in hospitals rather than hospice.”
Dying with or from cancer
Much like the fractious debate over COVID death certificates, describing health expenditures based solely on cancer mortality has significant and not mentioned limitations. Leave aside the debate over whether an individual dies with or from cancer and how they may be “coded” on a death certificate – we know that is flawed. But is death the best measure; after all, no one gets out of life alive. Wouldn’t it be better to talk not of the final endpoint but the length of time and the quality of our care or that of other countries? Aren’t quality adjusted life years (QALY) a better metric?
The individuals doing this research know that QALY is better, but that information is not available. So like the drunk searching for his car keys, they look under the nearest street lamp because the light is better there. But the conclusions they reach are not as useful. There are many reasons for our “excess” spending, not the least of which we believe that we can and should extend life, something that was not measured. One of the questions we might raise is whether some of those costs go to keeping the increasingly frail alive; certainly, our spending on “marginal or unclear survival gains” suggests that may well be the case.
[1] That is to say, for equivalent dollars, do you get more products in one country than in another.
Source: Comparison of Cancer-Related Spending and Mortality Rates in the US vs. 21 High-Income Countries JAMA Health Forum DOI:10.1001/jamahealthforum.2022.1229 (




