This week, a new study was discussed at a meeting of the Obesity Society and published in JAMA Network Open concerning the impact of Ozempic and other anti-obesity drugs on an individual’s intake of alcohol. I had noticed a decrease in my alcohol intake within a week or two of beginning the use of semaglutide, but the study confirms that I am not alone.
Using a cohort consisting of about 14,000 WeightWatchers engaged in their telehealth weight management program, the researchers asked about alcohol use before and after initiating treatment with a range of anti-obesity drugs. However, the overwhelming number (86%) used the headline-grabbing second-generation GLP-1s, e.g., Ozempic, Trulicity, and Monjauro. As you might anticipate from a WeightWatchers program, 86% were women, and the median age was roughly 43.
- 53.3% of participants indicated alcohol use at study initiation
- 24% of those participants indicated a decrease in alcohol use, and for nearly half of them (45%), the reduction was from one alcohol consumption category to another.
- 2.3% reported an increase in use
- Those drinking more or with greater initial weight reported were more likely to reduce alcohol consumption.
In my series of one, I have reduced consumption of alcohol significantly by roughly half and, like the cohort, lowered my alcohol consumption category.
Quantifying Alcohol Use
For researchers to quantify alcohol use, they must first agree upon what is considered a “standard drink.” It is based on the percentage of alcohol in the drink.
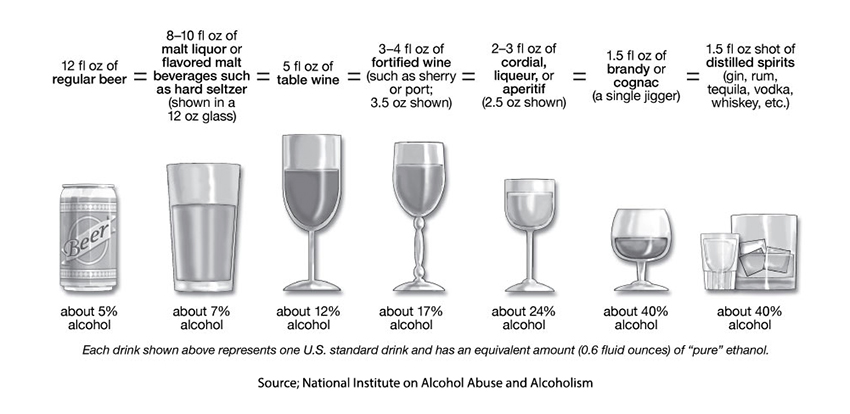
For the US, that is about 14 grams of alcohol. Cultural measures of a “standard” drink also vary from a low in Iceland of 8 grams to, unsurprisingly, 20 grams in Australia.
According to the Dietary Guidelines for Americans, intended to maintain our overall health and reduce chronic disease risk, and the CDC, moderate drinking is defined as 1 glass a day for the ladies and 2 for the men, basing that calculation on the differences in how they “process” alcohol. Given both a standard amount of alcohol ingested and a guideline for moderate drinking, we can theoretically, using math, determine an individual alcohol intake. Of course, none of these measures are hard and fast; they are all fuzzy – beer and wine have varying percentages of alcohol, and what constitutes a “glass,” especially when drinking at home, can go from a shot glass to a tumbler.
Further contributing to quantifying consumption is that physicians who record the information seem to feel that moderate drinking was 2.2 drinks/day, irrespective of gender. The categorization of drinking is further confounded because other ways of categorizing alcohol intake are based upon the risk of that drinking pattern resulting in alcohol use disorder. In this instance, low-risk drinking is no more than 3 drinks per day, 7 drinks per week for the ladies, 4 per day, and 14 per week for the men. Binge drinking is defined as four drinks in 2-hours for women and 5 for men. Heavy drinking is binge drinking on 5 or more days in a month.
The categorization in the current study did not fit into any of these standard groupings. [1] This makes the statement that anti-obesity drugs reduced drinking by a category, and therefore risk, difficult to use in comparing different research. This is one reason why research is not always reproducible; while the measurements remain the same, the categorization of those numbers varies.
Why?
We really do not have any answer, let alone a good answer, as to why the GLP medications reduce alcohol consumption, although it has been lumped in with GLP’s reduction in addictive behavior. Michelle I. Cardel, PhD, RD, Chief Nutrition Officer WeightWatchers and an author of the study suggests,
“What we hear from them is twofold, one, particularly amongst those folks on GLP-1 medications, we’re hearing that physiologically, they feel different with the medications, that their cravings for alcohol are decreased, and that when they do choose to drink that there’s often a very much a negative reinforcement…”
The other reason for drinking less in this situation is to free oneself of unnecessary calories. Alcohol by itself contains 7 calories per gram, but unless you are drinking ethanol, standard drinks contain other nutrients that add to their caloric load. A beer can contribute 146 calories, a glass of wine 159, and a shot of booze 61 calories. There are many calculators for drinks; you might try this one that not only tells you the number of calories but also provides the cheeseburger and exercise “equivalents.” (That beer is worth half of a cheeseburger). For those considerate moderate drinkers, stopping completely reduces your calories by a little more than a half-pound of weight loss during the week.
I found that the taste of wine was somehow “off” and that, as always, there was no need to drink “bad” wine. As my Ozempic journey shows, this medication isn’t just about the numbers on the scale; it’s about rethinking consumption—whether that’s food, drinks, or habits we once thought immutable. While science continues to explore the “why” behind these changes, I’ve found even small shifts can lead to surprising transformations. Whether it’s fewer drinks or fewer pounds, this journey is about redefining balance.
[1] “Category 0, no drinking; category 1,1 to 3 drinks for females and 1 to 6 drinks for males; category 2, 4 to 6 drinks for females and 7 to 14 drinks for males; category 3, at least 7 drinks for females and at least 15 for males.”
Sources: Alcohol Use and Anti-obesity Medication Treatment JAMA Network Open DOI: 10.1001/jamanetworkopen.2024.47644
Do Patients on Anti-obesity Drugs Decrease Alcohol Use? Medscape



