With COVID-19’s “public health emergency” barely behind us, lawyers and policymakers are taking advantage of public sensitivity and planning for the next plague. How good their solutions are remains to be seen, but novel suggestions, and attention to new technology and historical practices, are few and far between.
Last week in the New England Journal of Medicine, health law professor Lawrence Gostin outlined his proposals in an article entitled: The Origins of Covid-19 — Why It Matters (and Why It Doesn’t). Two of his three suggestions are reminiscent of those I previously wrote for ACSH and Harvard’s Bill of Health, a forum for health law policy and bioethical perspectives.
Professor Gostin’s assessment of possible epidemic sources as a launch point for future planning was particularly helpful. COVID could have emerged from:
- Natural causes: Natural zoonotic spillover, most likely at the Huanan Seafood Wholesale Market
- Lab leak at the Biosafety Lab in Wuhan
- Bioterrorism threat
It is impossible to categorically rule out the first two possible causes, and prudence dictates reducing potential exposure from all three.
“Of the three possibilities — natural, accidental, or deliberate — the most scientific evidence yet identified supports natural emergence.”
- Professor Larry Gostin and Dr. Gigi K. Grunval
While there are arguments for accidental or deliberate emergence, there is little doubt that COVID-19’s clinical expression began at the Huanan Seafood Wholesale Market.
Most pandemics (Asian flu, Hong King flu, Swine flu, SARs-1) have known animal origins. The mechanism for a plague virus’s development is generally attributed to genetic crossover or shifting from one species to another (species jumping) – the genetic “drift,” modifying genes. This mechanism has been attributed to the creation of the COVID-19 virus.
Why the sudden genetic changes?
One little-mentioned possibility is the consequences of natural disasters such as earthquakes, hurricanes, floods, and drought. When animals and humans live in close proximity, as they do in wet markets, the likelihood of species-jumping events during a period of natural havoc is magnified. As for the time it takes for new mutants to occur and take root in the population – that, as yet, is unknown.
What we do know is that the COVID-19 epidemic became apparent via a cluster of pneumonia cases in Wuhan in late fall of 2019 and that six months previously, a Grade 5.8 caliber earthquake struck the Chinese province of Sichuan, the site of the worst earthquake in Chinese history in 2008. The earlier earthquake tremors were felt 900 miles away. Wuhan is 600 miles from Sichuan. Is there any connection between the earthquakes and the development of the COVID-19 virus? Who knows? But perhaps research on the subject might be a good idea. As to how long the new virus was brewing before it took hold and manifested in the human pneumonia clusters - that too is unknown. Several months perhaps?
But one easily implemented prevention program might be an international monitoring registry of natural disasters near places where emergent disease organisms arose in the past or where dangerous microorganisms are known to be -for example, for research use.
Follow the Virus, Stop the Spread – Travel Advisories
In contrast to their response to SARS I, the WHO declined to issue travel advisories.
When the virus was limited to China, that response could be justified. Perhaps when its spread was limited to South Korea or Iran, the virus’ initial ports of call, that decision could be supported. But a world alarm should have sounded once the virus made port-of-call in Lombardy, Italy. How the virus was transported from China to Italy – and from there to the rest of the world- is hardly a mystery. And it could have been slowed or stopped by a travel ban, even by mid-January 2020.
COVID-19 attacked Lombardy (the province that contains Milan) smack during Milan fashion week, just as “strange cases” of pneumonia were noticed in the area. As photographic promotion for the event suggests, China is a prime player in the international fashion industry. The virus could have hitched a ride on a fashion model, fashionista-tourist, or a trunk full of clothes. Once it hit the runway of the nearby international fashion fair, it was only a short jump to the homes of other international fashion players: Spain, France, the UK, and the US - precisely the path the virus took.
Perhaps chastened by the exaggerated response to Ebola or in response to a newly freedom-focused or economically-prioritizing population, the WHO refused to issue such advisories for COVID. The US, similarly, played dumb to human-hopping viruses importing COVID across international boundaries.
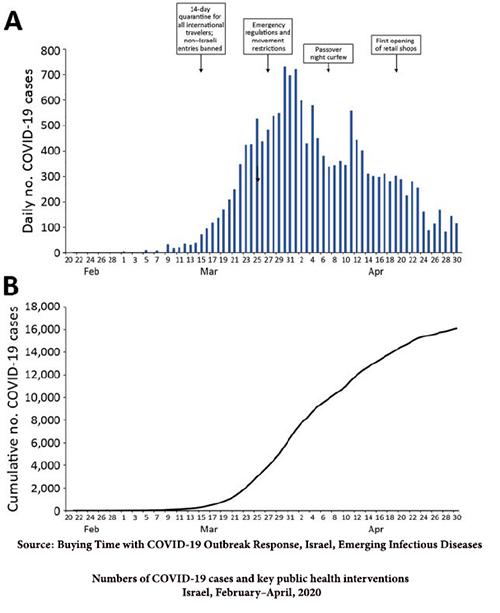
The impact of restricting international travel
Israel initially, and then intermittently, restricted international travel. Originally, Israel boasted low rates of infections, but once the airways opened, Israel’s early successes failed, and it began hosting some of the world’s highest infection rates, even as it boasted the highest vaccination rates.
Yes, this is only a correlation, but it is suggestive and indicative of effective measures that reduce the spread of the virus by reducing the movement of its hosts, us.
Prepare for the Worst - Environmental Monitoring
Exposure to epidemic pathogens is primarily via inhalation and secondarily by ingestion (eating and drinking). The third route, through skin contact, rarely poses a concern for pandemic spread, other than in rare cases where all three routes can cause disease, such as anthrax.
While airborne spread or person-to-person contact is typically the most common means of dispersal, fecal spread can also impact transmission. Even for airborne pathogens, such as SARs-1, environmental monitoring picked up viral particles where other epidemiological contacts couldn’t be identified. Wastewater (sewage) monitoring for COVID was first developed in September. 2020, months into the epidemic.
Both these methods, wastewater and air monitoring, can detect the presence of pathogens early and in the asymptomatic. Such screening measures should be instituted when a pandemic is first identified, but a validating protocol needs to be developed now to have it ready for when it might be required.
Generic Prevention
Prior to developing a specific treatment, antibody, or vaccine, which can only be done once the “organism-of-interest” has been identified and genetically- sequenced (after it’s been fingered on the scene), general across-the-board protectants are usually limited to masking in cases of airborne transmission.
Research on effective masks should be done now to evaluate prevention potential based on particle (or droplet) size and sample pathogens. Currently, the most effective use requires masks to be fit-tested – i.e., molded to one’s face; facial hair also impedes effectiveness. Is there a design change that could reduce that need? The most efficient masks (typically N99 or N95) should be stockpiled for emergency use- by everyone, not just health care providers. Research could also be done on effective, efficient, and rapid means of production, such as 3-D printing, to quickly replace reserves during a pandemic.
- Public information campaigns should be in place to alert the public of good-masking practices. Such preventative planning might have obviated the "any-bandana-will-do-ya advice" that went viral at various phases of the pandemic.
Finally, pneumonia clusters have been the “canary” response to all modern pandemics. And while government hiding of epidemic information is neither new nor limited to China [1], it is difficult to prove till too late. Requiring public disclosure of pneumonia clusters (together with draconian UN sanctions) might be a good start to international pandemic preventiveness.
[1] International transport of pandemic pathogens has long been recognized – and feared. In the last centuries, the US had special consuls in all countries with which the US had contact to prevent ships laden with disease-exposed passengers from embarking for the US. In 1892, several ships laden with cholera carriers left without the special consul being notified of an epidemic at the port of embarkation. The country at fault: Germany.