
Despite declining mortality rates, cardiovascular disease affects approximately 47.8 million women in the United States, while breast cancer affects about 3.3 million. Breast cancer receives far greater public attention, yet cardiovascular disease accounts for 1 in 3 deaths among women, compared with roughly 1 in 31 deaths from breast cancer. Advances in early detection and treatment have created a growing population of nearly 3 million breast cancer survivors. Today, almost 90% of patients survive at least five years after diagnosis, and more than half of survivors are over age 65, a demographic shift that fundamentally changes long-term health priorities.
This growing population of older survivors sets the stage for a paradox that only becomes apparent years after cancer treatment ends.
The Survivor’s Paradox: Unintended Consequences of Cancer Success
Our success in treating breast cancer has introduced a new clinical challenge. As women survive their initial cancer diagnosis, they increasingly face long-term cardiovascular complications. In fact, breast cancer survivors are more likely to die from cardiovascular disease than from a recurrence of their cancer. Many of these cardiac threats emerge years after treatment ends, particularly among older, postmenopausal women, whose risk of cardiovascular death eventually exceeds that of women without a history of breast cancer.
Why does surviving breast cancer so often come with an increased risk to the heart?
The Influencers
Age is a primary determinant of a survivor's subsequent health path. While the incidence of breast cancer doubles every decade until menopause, the risk of CVD accelerates sharply thereafter. Racial and ethnic disparities further complicate this picture. Black women are more likely to develop breast cancer before age 45 and to be diagnosed at later stages, which worsens cancer outcomes. They also experience higher cardiovascular mortality.
Beyond age and demographics, breast cancer and cardiovascular disease are linked by shared biological and behavioral risk factors.
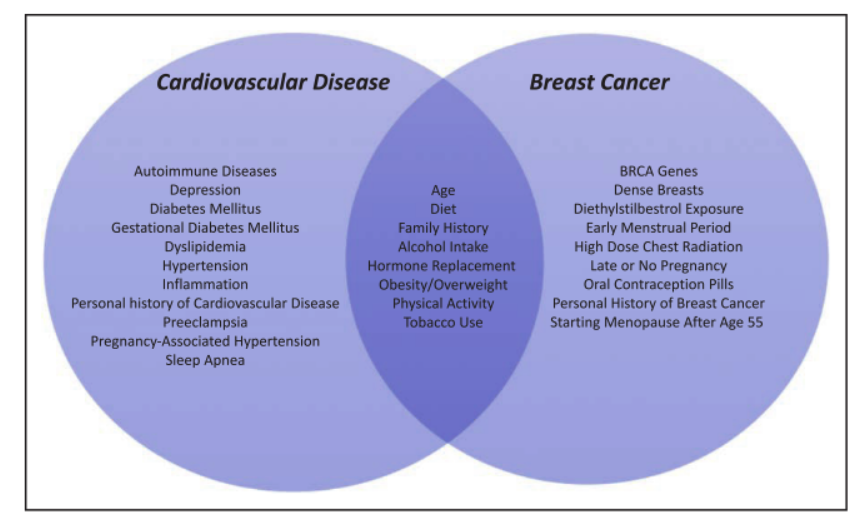
- Dietary patterns: Diets rich in vegetables, fruits, and whole grains are consistently linked to lower cardiovascular mortality, while evidence for breast cancer prevention remains mixed.
- Alcohol consumption: Although alcohol has been debated for possible cardioprotective effects, the American Heart Association emphasizes that it offers no cancer-related benefits.
- Physical activity: At least 150 minutes of moderate exercise per week reduces mortality from both diseases. Prolonged sitting—more than 10 hours per day—raises cardiovascular risk and is associated with higher breast density, a marker linked to breast cancer.
- Obesity: Obesity is a major driver of cardiovascular disease. Its relationship with breast cancer depends on menopausal status, increasing risk after menopause, but paradoxically reducing risk before menopause.
- Tobacco use: Smoking is a major cardiovascular risk factor, though its association with breast cancer is weaker.
- Hormonal timing: Early menopause increases cardiovascular risk but lowers breast cancer risk, while late menopause substantially increases breast cancer risk.
- Genetics: Variants such as BRCA1 and BRCA2 increase cancer risk and may also influence susceptibility to chemotherapy-related heart injury.
It is this final factor, the cardiovascular effects of breast cancer treatment, that most directly underlies the survivor’s paradox. For many survivors, there is an unintended race between two diseases. Gains in cancer survival can be undermined by radiation-induced atherosclerosis, chemotherapy-related heart failure, or cardiovascular risks that received less attention during active cancer treatment.
Long-term population studies help illustrate how this risk unfolds over time.
Tracking Survivors Over Time
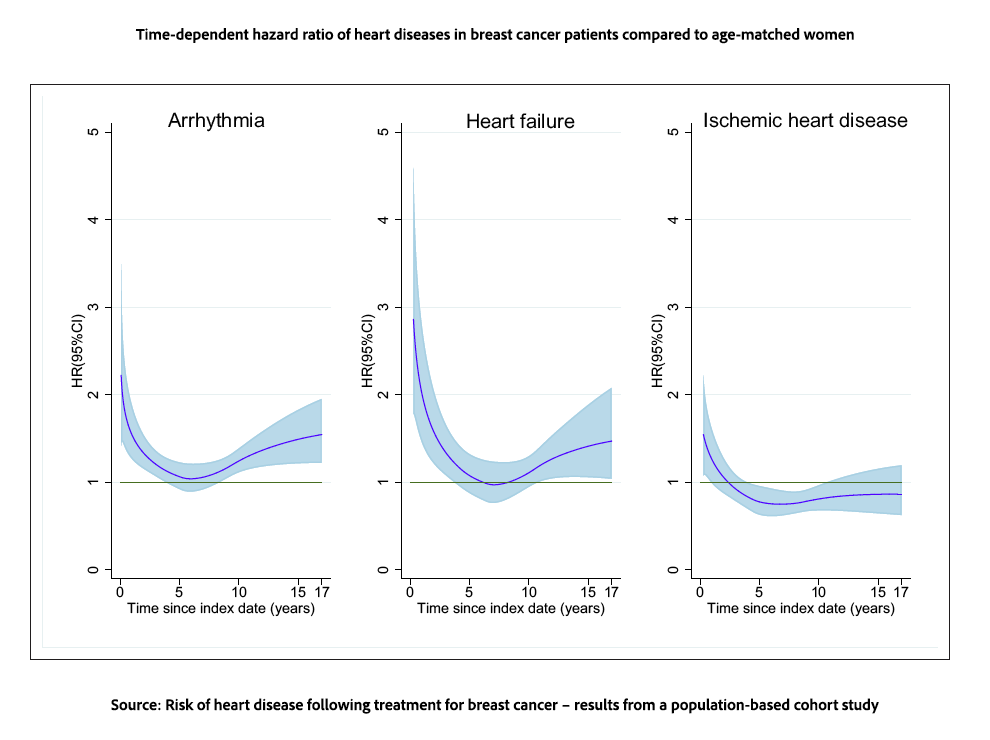
A longitudinal study of Swedish women followed 8000 women in the Stockholm-Gotland Breast Cancer Registry without a prior history of heart disease, and compared them with a random sample of women from the general population matched on year of birth. The women, with a median age of 59, were followed for a median of roughly 11 years. Primary treatment included surgery and/or radiation therapy. 80% received adjuvant hormonal therapy, 40% received adjuvant chemotherapy.
At 10 years, breast cancer patients had a greater incidence of arrhythmias and heart failure, while the incidence of ischemic heart disease was essentially the same. Radiation therapy is known to promote accelerated atherosclerosis and microvascular injury. In women undergoing radiation therapy, those being treated for a left-sided breast cancer (over the heart) had a non-significant increase in ischemic heart disease compared to those with right-sided cancers. As the American Heart Association notes, this cardiovascular risk remains elevated for up to 30 years post-exposure.
“In a population-based setting, we demonstrated that the incidence of heart disease in breast cancer patients was significantly higher than the incidence observed in matched reference individuals from the general population. The risks of arrhythmia and heart failure were increased even beyond 10 years after diagnosis.”
The researchers suggested that the increased risks of arrhythmia and heart failure were related to the cardiotoxic effects of chemotherapy on the heart muscle, myocardium, with no impact upon the coronary vessels themselves. [1] The subsequent lower-term risk of ischemic heart disease may reflect another, previously mentioned risk factor now paradox: in general, women with longer exposure to estrogen, earlier menarche, and later menopause have an increased risk of breast cancer and a decreased risk of ischemic heart disease.
From Detection to Prevention
Current clinical approaches aim to detect subtle heart injury before symptoms appear, using advanced imaging and blood-based biomarkers.
One key tool is myocardial strain imaging, an ultrasound-based technique that detects subtle changes in how heart muscle fibers shorten and stretch. These changes often appear before conventional measures of heart function decline. When combined with elevated troponin I levels, itself a sensitive blood marker of heart muscle injury, clinicians can predict future cardiotoxicity with high accuracy.
In addition to oncologists searching for more cardioprotective chemotherapies, several cardiovascular medications are being investigated for their potential "dual-purpose" roles in preventing both heart injury and cancer progression. Patients, in addition to treating underlying hypertension and diabetes, can alter their diet and physical activity – cornerstones in mitigating the risk of CVD.
Greater recognition of the survivor’s paradox has already begun to change care. Survivorship programs now identify individuals at higher risk of cardiotoxicity [2], and post-treatment protocols increasingly include baseline heart evaluations followed by regular reassessment.
Heart-Conscious Cancer Care
The survivor’s paradox forces us to rethink what it truly means to be a breast cancer survivor. Survival is more than years free of recurrence. As the population of breast cancer survivors continues to grow, so does the responsibility to ensure that survivorship does not come at the cost of heart health.
Greater awareness is essential, pairing breast cancer treatment with vigilant cardiovascular monitoring, prevention strategies, and lifestyle interventions that protect survivors for decades beyond remission. Recognizing the heart as part of the survivorship journey is not an option. Surviving cancer should not mean succumbing to the disease we failed to see coming.
[1] Anthracyclines, chemotherapeutic agents, are a primary concern because they cause irreversible myocyte damage without a truly “safe dose” threshold. Other chemotherapeutic agents cause bradycardia, a slowing of the heart rate. In short, modern endocrine therapies entail a complex trade-off in terms of survival.
[2] Patients receiving doxorubicin (an anthracycline) at doses exceeding 240 mg/m² or thoracic radiation exceeding 30 Gy.
Sources: Cardiovascular Disease and Breast Cancer: Where These Entities Intersect Circulation DOI: 10.1161/CIR.0000000000000556
Risk of heart disease following treatment for breast cancer – results from a population-based cohort study eLife DOI: 10.7554/eLife.71562.sa0



