I’ve wondered about that last question for some time. Hypertension is a recognized COVID-19 co-morbidity, but a large portion of the population has hypertension; it didn’t seem to be a significant discriminator between little and lots of risk. And I haven’t seen a paper, pre-print or peer-reviewed, that showed co-morbidity’s relative impact. The data seems hidden in plain sight.
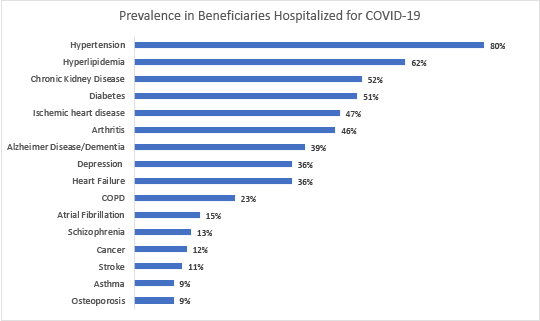 The Centers for Medicare and Medicaid Services (CMS) publishes a snapshot on COVID-19 and its beneficiaries, the latest reporting the cumulative results from January through mid-July. It can be found here. But this graph to the right is the top 16 co-morbidities for hospitalized patients. Before continuing, a quick caveat, the first of several. The beneficiaries here are those who have “traditional” Medicare or fee-for-service care; it does not represent the 38% of beneficiaries that use a Medicare Advantage program. [1] As you can see, hypertension and its fellow traveler hyperlipidemia are by far and away the greatest risk factors. Or are they? The difficulty with the simple interpretation of this data is that while we have numerators, like the percentage of COVID hospitalizations with diabetes, we do not have the denominators, how many beneficiaries, with and without hospitalization, have diabetes. That information can be found in a different CMS dataset, which can be found here.
The Centers for Medicare and Medicaid Services (CMS) publishes a snapshot on COVID-19 and its beneficiaries, the latest reporting the cumulative results from January through mid-July. It can be found here. But this graph to the right is the top 16 co-morbidities for hospitalized patients. Before continuing, a quick caveat, the first of several. The beneficiaries here are those who have “traditional” Medicare or fee-for-service care; it does not represent the 38% of beneficiaries that use a Medicare Advantage program. [1] As you can see, hypertension and its fellow traveler hyperlipidemia are by far and away the greatest risk factors. Or are they? The difficulty with the simple interpretation of this data is that while we have numerators, like the percentage of COVID hospitalizations with diabetes, we do not have the denominators, how many beneficiaries, with and without hospitalization, have diabetes. That information can be found in a different CMS dataset, which can be found here.
Before moving on, our second caveat. This data is the latest from CMS but is for the year 2017, and it covers all of Medicare’s beneficiaries, including those in Medicare Advantage programs. So, the next calculation is based on my assumption that the prevalence of co-morbidities changes only slightly over time – that 2017 is representative of 2020; and that beneficiaries in Medicare Advantage, for their co-morbidities, are pretty much the same as those using traditional Medicare.
There are any number of ways to introduce the denominator into our calculations, such as hazard, and relative risk ratios. For this observation, I simply used the reported 2017 prevalences as the denominators. Values of 1 mean that co-morbidity was equal in both populations – the co-morbidity did not seem to create a greater risk of hospitalization. Values of less than 1 imply the co-morbidity imparts some protections, while values greater than 1 indicate enhanced risk. The further away from the baseline of 1, the greater the effect. Here are the results after correcting the underlying prevalence of a co-morbidity in the population.
A much different picture emerges
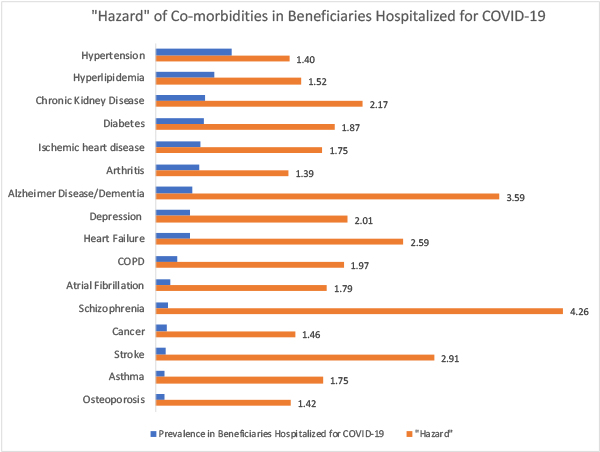 As a physician, I would have thought that the respiratory illnesses, COPD, and asthma would rise in the rankings, and I might have guessed that heart failure and chronic kidney disease would be up there too. But look at the two chronic conditions that pose the most significant risk, schizophrenia and dementia followed closely in third place with stroke. I see no bio-plausible pathway for these conditions to be the significant drivers of hospitalization. Well, that is not entirely true. I suspect that these three conditions are associated with a higher incidence of institutionalization; for these patients to be more likely to reside in chronic care facilities. And we have data on the harmful relationship between long-term facilities and COVID-19.
As a physician, I would have thought that the respiratory illnesses, COPD, and asthma would rise in the rankings, and I might have guessed that heart failure and chronic kidney disease would be up there too. But look at the two chronic conditions that pose the most significant risk, schizophrenia and dementia followed closely in third place with stroke. I see no bio-plausible pathway for these conditions to be the significant drivers of hospitalization. Well, that is not entirely true. I suspect that these three conditions are associated with a higher incidence of institutionalization; for these patients to be more likely to reside in chronic care facilities. And we have data on the harmful relationship between long-term facilities and COVID-19.
A final caveat, co-morbidities rarely travel alone, and prevalence does change, in some cases, with ethnicity. Schizophrenia is the sole chronic condition for about 9% of Medicare beneficiaries and is found in 45% of beneficiaries that have five or more chronic conditions. Dementia is a less common stand-alone, at roughly 4.5%, but it has more traveling companions, with 53% of beneficiaries reporting dementia along with four or more other chronic conditions.
I will leave it to my academic peers to tease out the deeper connections here. But I have demonstrated the importance of looking at numbers within a context; no number stands alone. What we perceive as a risk in COVID-19 changes dramatically when we apply context. And hopefully, I have opened the possibility that those of us with chronic conditions can begin to appreciate our individual risk and let the data reduce our fears. Does having elevated cholesterol and blood pressure increase your risk? Yes. But nowhere to the degree that other conditions do and certainly not to the degree that you remained locked up, fearful of going outside, scrubbing your packages.
[1] Fee-for-service accounts for 62% of Medicare beneficiaries, roughly 54.5 million individuals.




