There is an urgent need for research in the area of pain management. Since the 1890s, when aspirin and heroin were discovered, there has been agonizingly little progress in this field. Some would argue that introducing Tylenol (acetaminophen, paracetamol, APAP, others) in 1950 represents progress. I would argue with them. As I wrote in a review of the drug's pros and (mostly cons) (See Tylenol Isn't So Safe, But At Least It Works, Right?), there are precious few painful conditions for which the drug works, and many more where it does not. It would be one thing if the drug had even a modest effect but was generally safe to take. But this is false (See Is Tylenol 'By Far The Most Dangerous Drug Ever Made?')
Nonetheless, Johnson & Johnson's Tylenol analog, JNJ-10450232 (1), now undergoing clinical trials, is being touted as a much safer alternative to Tylenol. Are they onto something? Let's look.
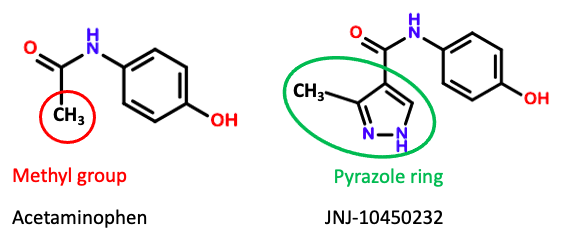
Figure 1. The chemical structures of acetaminophen and JNJ-10450232. Good luck finding the latter (2).
Finding a safer Tylenol-like drug should not be difficult. This is because acetaminophen itself is not toxic; but the drug undergoes oxidation by the liver, and its metabolite NAPQI is highly hepatotoxic (Figure 1). It is NAPQI that destroys the liver. A comparible drug that does not undergo this oxidation would undoubtedly be safer.
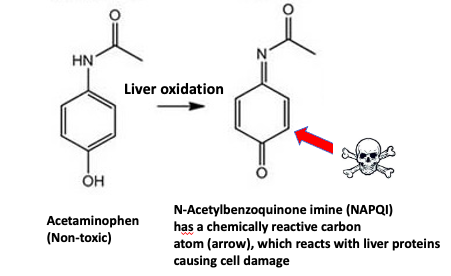
Figure 1. Acetaminophen undergoes rapid oxidation in the liver, forming a toxic metabolite responsible for the drug's toxicity. The red arrow indicates the reactive carbon that undergoes reactions with biomolecules (especially those that contain a thiol (-SH) group, causing severe liver damage.
Acetaminophen overdose is the leading cause for calls to Poison Control Centers (>100,000/year) and accounts for more than 56,000 emergency room visits, 2,600 hospitalizations, and an estimated 458 deaths due to acute liver failure each year. (3)
Source: Hepatology, 2004 Jul;40(1):6-9. , DOI: 10.1002/hep.20293
Is this progress?
JNJ-10450232 is discussed in a paper published in the journal Regulatory Toxicology and Pharmacology. The article is a bit sparse on details, so we will have to make a few assumptions. The paper's first sentence is not encouraging [emphasis mine].
JNJ-10450232 (NTM-006) is a new molecular entity that comprises structural similarities to acetaminophen and provides comparable analgesia in animals and humans without causing the hepatotoxicity associated with acetaminophen overdose in preclinical models.
Source: Kuffner, et. al., Regulatory Toxicology and Pharmacology, Volume 134, October 2022, 105236.
Well, that's not a great start. J&J succeeded in solving one of the two problems with acetaminophen – its toxicity. Unfortunately, "comparable analgesia" kind of blows up the safety solution since it doesn't matter how safe a drug is if it doesn't work. In a sense, JNJ-10450232 can be viewed as a "safer placebo."
Improved safety
At single doses as high as 6,000 mg – twice the recommended daily maximum of Tylenol – JNJ-10450232 had a half-life of 8-10 hours (this is good), and no dose-limiting toxicity was observed (also good). The only common side effect was a skin rash. The highest multiple-day dose studied – 2,500 mg twice daily for eight days was not problematic. The clinical toxicology profile of JNJ-10450232 is clearly superior to that of Tylenol. One should not take 5,000 mg of Tylenol daily for eight days.
Why the improved safety? I can only guess that JNJ-10450232 is not a substrate for CYP2E1, the primary liver enzyme responsible for converting Tylenol to NAPQI, the toxic metabolite, perhaps because of the size of the pyrazole group.
But does it work? (emphasis mine)
There is no way I can look at this drug, especially without more complete data, and find any reason to be optimistic.
JNJ-10450232 (NTM-006) is a new molecular entity that has structural similarities to acetaminophen (Fig. 1). In rodent pharmacology models, it exhibits similar antinociceptive [pain blocking] and antipyretic [fever reducing] effects to that of acetaminophen and shows potential to have a longer duration of action.
Source: Kuffner, et. al., Regulatory Toxicology and Pharmacology, Volume 134, October 2022, 105236.
Here are a few quotes showing why the above statement is discouraging.
However, in this network meta-analysis, the most remarkable result is that paracetamol does not seem to confer any demonstrable effect or benefit in osteoarthritis, at any dose. This finding is not entirely unexpected. Paracetamol has been on the market for as long as most of us remember. Its efficacy has never been properly established or quantified in chronic diseases and is probably not as great as many would believe. Its safety is also questioned, not just in overdose. Is recommending it as the universal first-line analgesic in osteoarthritis still tenable?
Dr. Nicholas Moore Department of pharmacology,University of Bordeaux France The Lancet, VOLUME 387, ISSUE 10033, P2065-2066, MAY 21, 2016, DOI:https://doi.org/10.1016/S0140-6736(15)01170-8
"It's an old drug, obsolete, and should be avoided altogether."
Kay Brune, a professor of pharmacology and toxicology at Germany's Friedrich-Alexander University
The addition of 1 g of IV acetaminophen to 1 mg of IV hydromorphone provided neither clinically meaningful nor statistically superior analgesia than hydromorphone alone.
Bijur, et. al., Academic Emergency Medicine, 20 February 2020 https://doi.org/10.1111/acem.13947
Finally, from ACSH friend Dr. Aric Hausknecht, a New York neurologist and pain management physician:
In my clinical experience, acetaminophen is a second-tier medication for mild to moderate pain. NSAIDs are first-tier but are contraindicated or not well-tolerated by some patients. Acetaminophen has very limited utility for moderate to severe pain, chronic pain or neuropathic pain. Additionally, the short half life limits and potential hepatotoxicity are limitations.
Although these opinions do not represent an undisputed or unbiased consensus on Tylenol's utility or shortcomings, they should not be dismissed. Thousand of pain patients have found Tylenol to be useless. Many have written to me saying just this. It would seem that Neumentum (this is where the name NTM-006 comes from), the company that licensed JNJ-10450232 from J&J, may regret this decision. Are people really going to want to spend X (X = many) of dollars on a new prescription drug that will enable them to take more of a similar medicine that doesn't work any better.
I just don't see it.
NOTES:
(1) NTM-006 is the name given by Neumentum, the company that licensed JNJ-10450232 from J&J. I wish them luck. They're gonna need it.
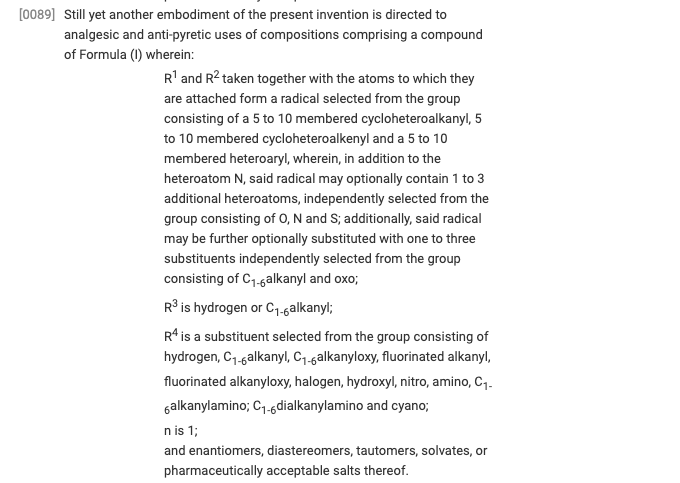
(2) Sometimes, it is nearly impossible to find a drug's chemical structure, even one in clinical trials. Companies may keep the structure secret to avoid attracting competitors that can modify the drug's formula to enable them to launch a copycat program. This was no exception. I spent hours looking for the damn thing and finally found it in a patent. (And the JNJ number isn't specifically named in the patent; I had to infer it from the claims.) Ever try reading a patent? Here's a snippet of what I had to go through to finally find the damn things. Those experiencing suicidal ideation should skip this.
(3) While 458 deaths may not seem like a large number, this is misleading. It is the number of 50,000 emergency room visits that is more telling. If caught in time, Tylenol poisoning can be successfully treated by an antidote called N-acetylcysteine. If not for the antidote, the number of deaths would be much higher.