The wellness world’s latest fixation is glucose spikes. Influencers like Jessie Inchauspé, aka the Glucose Goddess, have convinced millions that flattening blood sugar “curves” is key to optimal health.
Inchauspé’s Glucose Revolution claims that post-meal glucose spikes cause a laundry list of problems, from brain fog to wrinkles and even cancer. For healthy people, her glucose-smoothing hacks contain some kernels of scientific truth, but are mostly solutions in search of a problem.
Blood Sugar Is Meant to Fluctuate
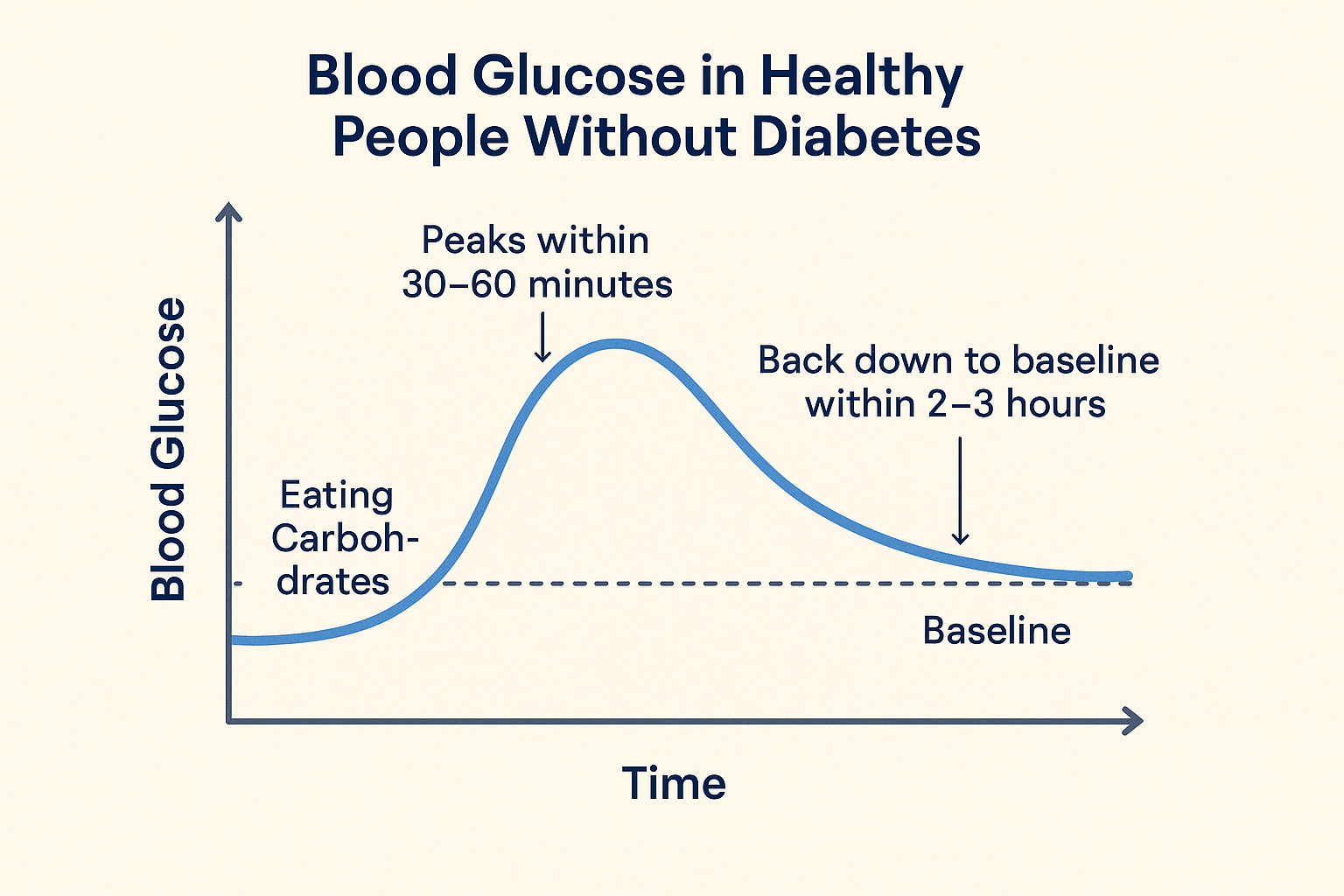 In healthy individuals without diabetes, blood glucose levels usually peak within 30–60 minutes after consuming carbohydrates. Then insulin brings it back down to baseline within two to three hours. The size of the curve depends on what and how much you eat, but the rise and fall are a normal metabolic response.
In healthy individuals without diabetes, blood glucose levels usually peak within 30–60 minutes after consuming carbohydrates. Then insulin brings it back down to baseline within two to three hours. The size of the curve depends on what and how much you eat, but the rise and fall are a normal metabolic response.
Chronically high glucose, as seen in diabetes, is a problem—but brief spikes are just your body doing its job.
A 2019 study found that healthy, nondiabetic individuals spent a median of 96% of the time in the “ideal” blood glucose range (70–140 mg/dL) when tracked with continuous glucose monitoring (CGM). No surprises there—the body is remarkably good at keeping glucose within tight limits.
CGMs Create Unnecessary Anxiety
Alongside the rise of blood sugar influencers, there’s been a considerable uptick in the use of continuous glucose monitors by people who don’t need them—namely, those without diabetes.
In theory, CGMs may have value for individuals at an increased risk of diabetes if they aid in early detection or prevention. They’ve also been touted as offering potential performance benefits for elite athletes. But even in these cases, solid evidence is lacking.
More concerning is that CGM use can fuel anxiety: users may misinterpret normal spikes as a problem and start fixating on “perfect” glucose levels, which risks disordered eating. Obsessive attention to smoothing out glucose levels can even lead some people to eat unnecessary extra calories when their glucose levels naturally dip.
Are Any Glucose Hacks Worth Trying?
That said, regularly experiencing rapid rises in blood sugar isn’t ideal. A 2018 PLOS Biology study found that even individuals with reasonable long-term glucose control may experience post-meal spikes into the prediabetic (140–199 mg/dL) or even diabetic (≥200 mg/dL) range. Although the long-term health impact of these transient excursions remains unclear, it’s likely beneficial to try to reduce the impact of high glucose peaks, which place greater demand on insulin production. The evidence isn’t settled, but over years, this could contribute to insulin resistance in susceptible people.
Eating vegetables and protein first, drinking vinegar before meals, avoiding oats, and never consuming fruit juiced or blended are some of Inchauspé’s oft-repeated hacks for blunting glucose peaks. Most are joyless gimmicks; however, a couple aren’t complete nonsense.
The best evidence-backed strategy for moderating glucose is to move rather than slump on the couch. A small study found that a 10-minute walk immediately after consuming a glucose load reduced peak blood glucose levels by about 10% in healthy young adults compared to resting. A 2022 meta-analysis found that 2–5-minute light-intensity walks every 20–30 minutes during periods of prolonged sitting significantly lowered post-meal blood glucose levels in overweight and obese adults.
Another hack espoused by the Glucose Goddess—what she calls ‘clothes on carbs’—is simply (pun intended) a dressed-up version of common-sense nutrition: eat carbohydrates alongside other macronutrients as part of a balanced meal. Nutrition science supports this, as pairing carbs with protein, fat, and fiber slows digestion and helps moderate glucose peaks.
Skip the Sensors: Get Your HbA1c Checked
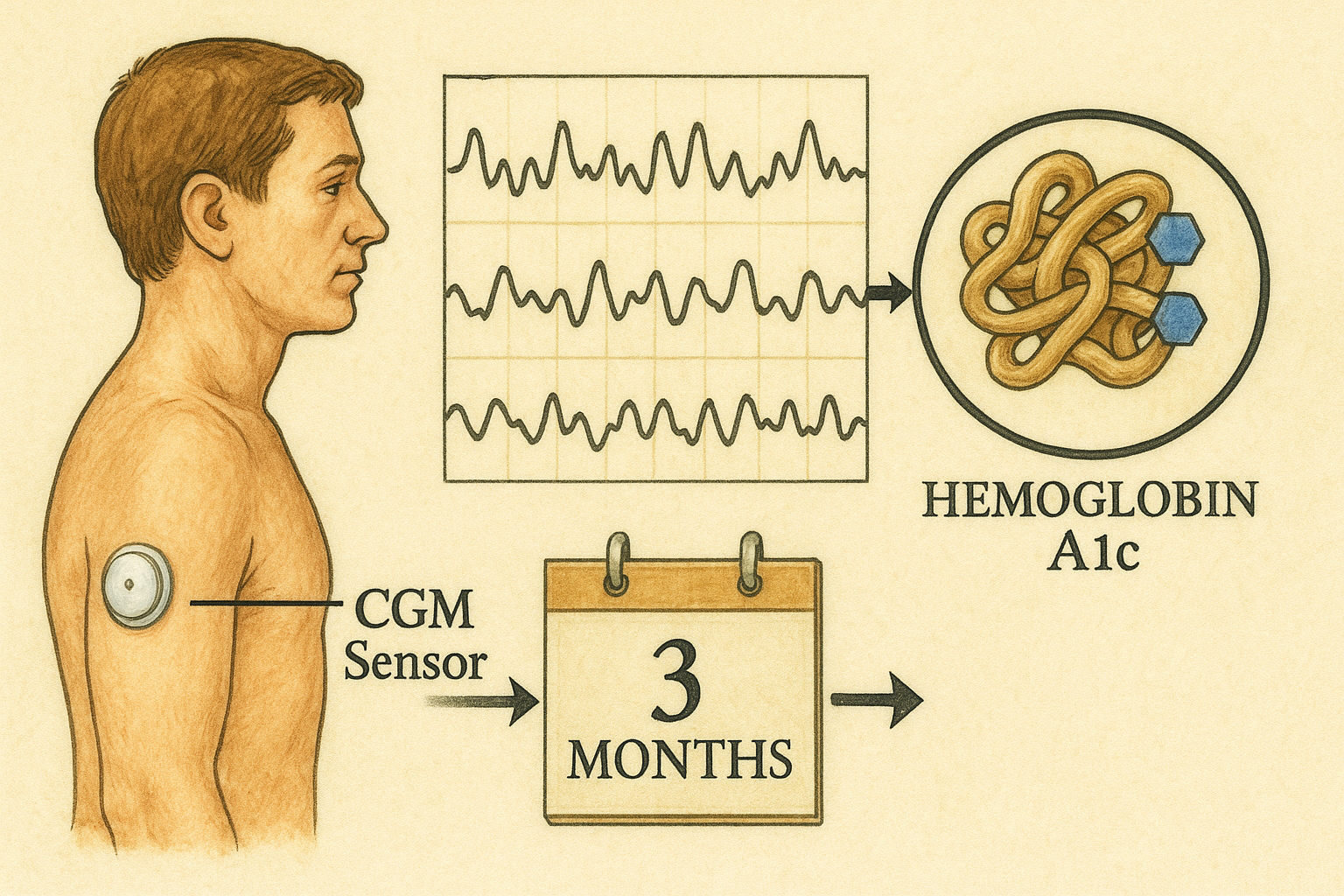 Instead of wearing a pricey sensor and panicking over every upward glucose shift, the most straightforward way to check if your glucose control is healthy is the HbA1c blood test.
Instead of wearing a pricey sensor and panicking over every upward glucose shift, the most straightforward way to check if your glucose control is healthy is the HbA1c blood test.
HbA1c checks the percentage of hemoglobin (the oxygen-carrying pigment in red blood cells) that has glucose attached to it. Since red blood cells last around three months, this test indicates your average blood sugar levels over this longer period. It makes it a reliable way to see your long-term glucose control, without getting hung up on daily ups and downs
For most healthy adults, a normal HbA1c is below 5.7%. Levels between 5.7–6.4% suggest prediabetes, and 6.5% or higher is diagnostic for diabetes (though always interpret your own levels with the help of a health professional).
Unlike CGMs, HbA1c captures the long-term picture—the one that really matters for metabolic health and future risk. It’s not expensive, available through your GP, and recommended every three years, or more often if you have risk factors for diabetes such as family history, being overweight, or high blood pressure.
The bottom line? Instead of chasing “perfect” glucose curves, focus on simple, sustainable habits: take a short walk after meals, eat regular, balanced meals, and avoid oversized portions. And for peace of mind, check your HbA1c—it’s a proven, no-nonsense way to monitor metabolic health without the hype.



