Men’s mental health changes with age—but not always for the reasons people assume. While hormones matter, they’re only part of a bigger picture. How testosterone’s shifts impact men will help men, their partners, and clinicians choose the right next step.
When “Not Myself” Becomes the Norm
A man in his late 40s tells me he’s “not himself”—sleep is lighter, patience thinner, libido lower, workouts stalled. He isn’t in crisis, but he’s quietly struggling. Another client in his 60s reports new irritability and “brain fog,” especially after poor sleep or high-stress weeks. In both cases, a comprehensive check of mood, sleep, medical conditions, medications, and hormone patterns clarified what to change and what not to chase. For many men, mood and motivation reflect a tug-of-war between aging biology, life stress, sleep, and health conditions, not the single-number, “low T” story.
The Hormone Landscape: Beyond Testosterone
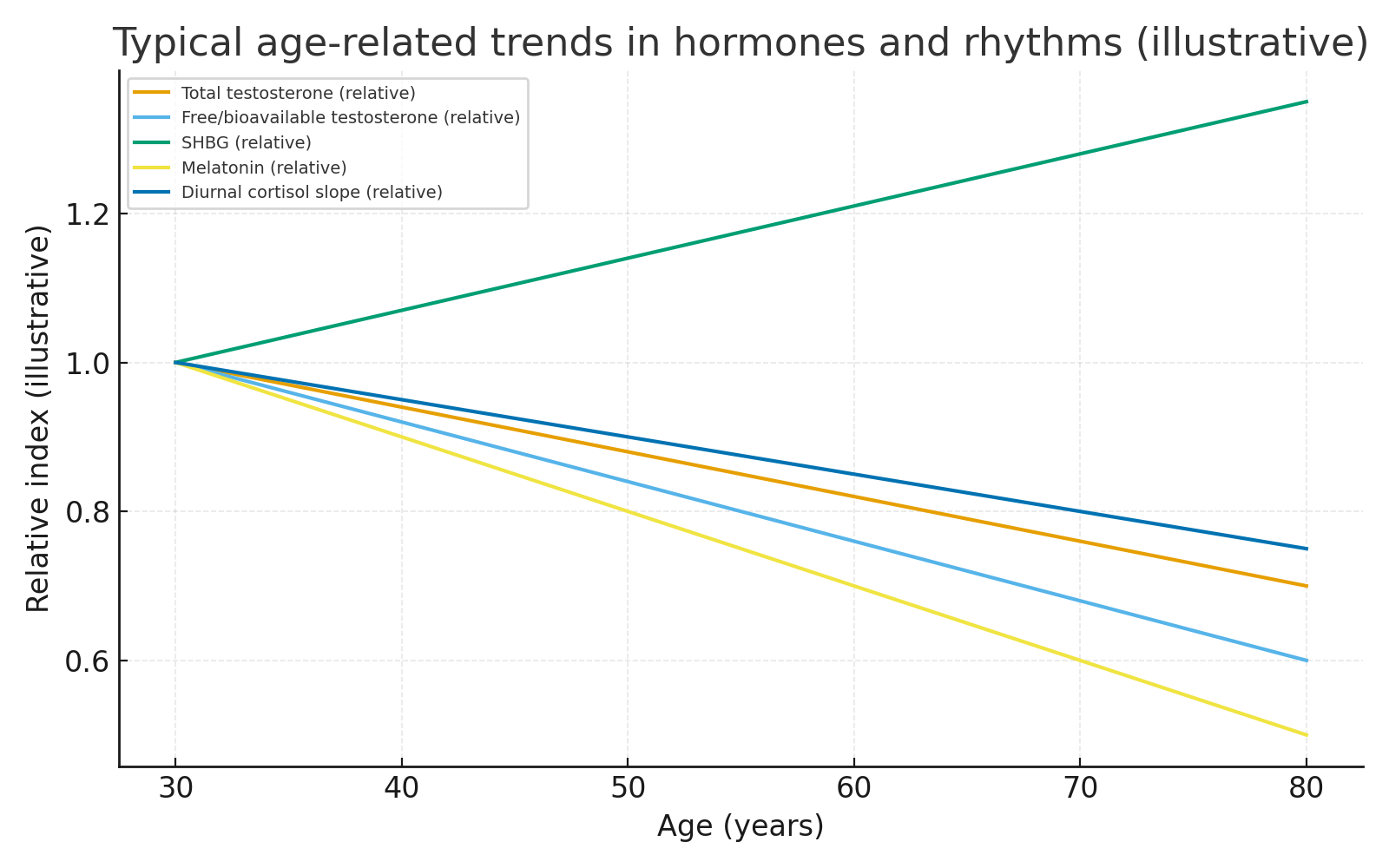
Testosterone (T) levels typically decline with age, while a protein called sex hormone-binding globulin (SHBG) tends to rise. This matters because SHBG binds to testosterone, reducing the amount of "free" or bioavailable T your body can actually use. Large studies such as the Baltimore Longitudinal Study of Aging and the European Male Ageing Study have documented these trends, with bioavailable T showing the clearest downward trend.
Other hormones are also in play:
- Estradiol (E2): In men, this hormone is derived from the conversion of testosterone in fat (adipose) tissue. As body fat increases, this conversion process can become more active, altering the crucial testosterone-to-estradiol balance, enhancing estradiol and influencing energy, libido, and body composition.
- Circadian & Stress Hormones: The systems that regulate sleep and stress also change. Melatonin production typically declines with age, and the body's core stress-response system can show flatter cortisol rhythms. Both can affect sleep quality, energy, and emotional regulation.
As these hormones shift, men may notice low mood, irritability, fatigue, brain fog, and reduced stress tolerance.
Depression is multifactorial; biology, life context, and health behaviors all contribute. Hormones are contributors, not the whole cause.
What the Evidence Really Says
- Testosterone & mood. Randomized data suggest testosterone treatment can reduce depressive symptoms in select men, but trials are heterogeneous and depression is rarely the primary endpoint. In short: there’s a signal, not a cure-all.
- Cardiovascular safety context. The TRAVERSE trial found that testosterone therapy did not increase major adverse cardiac events in middle-aged or older hypogonadal men with CV risk factors. Regulators later updated product labels to add blood pressure warnings based on ambulatory BP studies.
- Thyroid & mood. Thyroid dysfunction can mimic or worsen depression; reviews show associations between abnormal thyroid function and depressive symptoms, but these associations ≠ automatic causation. Thyroid disease should be treated when indicated, but it is rarely the single driver.
- Sleep apnea & testosterone. Obstructive sleep apnea (OSA) is linked to lower testosterone levels; addressing OSA can improve daytime energy, cognition, and mood, and avoid blaming everything on “hormones.”
- Lifestyle and environment: Chronic sleep restriction, high stress, heavy alcohol use, inactivity, and certain medications (e.g., opioids and some antidepressants) can worsen the picture. A medication and sleep screen often clarifies first steps before any hormone therapy is considered.
Testing Smart Without Chasing Numbers
Professional guidelines converge on two points: diagnose testosterone deficiency only when both signs/symptoms fit and lab data show consistently low levels measured correctly. Measure fasting morning total testosterone. If total T is borderline or SHBG is abnormal, obtain free T values. While the American Urological Association considers <300 ng/dL a reasonable total T cutoff supporting the diagnosis, it is a guide, not a one-number truth for every patient. Don’t treat age alone; the guidelines discourage routine testosterone therapy for asymptomatic age-related low T. Decisions should be individualized after discussion of benefits/risks and careful monitoring.
Your Action Plan: First-line moves that reliably help mood (with or without TRT)
- Map Your Symptoms: Keep a 2–3 week log of sleep, energy, mood, libido, alcohol use, and stressors. Patterns often point to the first and best place to intervene.
- Fix sleep and circadian drift. Target 7–9 hours, with a regular wake time. Melatonin physiology changes with age, causing a drift in your sleep pattern. Behavioral anchors often help the most.
- Train the body. Progressive resistance + aerobic activity improve energy, sleep, and mood; they also support metabolic health, favoring a better androgen–estrogen balance.
- Address stress physiology. Structured stress-reduction, e.g., problem-solving therapy or brief mindfulness, can improve mood and may help normalize stress-hormone rhythms over time.
- Rule Out the Obvious: Get a proper screening for depression and anxiety. Review medications (opioids and sedatives can suppress hormones). Consider a sleep apnea screening if you snore heavily or have significant daytime sleepiness.
- When indicated, thoughtfully order labwork: Start with the basics: morning total T tests, tests of luteinizing and follicle-stimulating hormones to classify the type of T deficiency, and, if symptoms warrant, targeted thyroid tests. Avoid expensive, unnecessary "shotgun" hormone panels.
- Plan for Tough Days: Men have higher suicide death rates than women. Create a brief crisis plan: know who you can call or text and when to seek immediate help (988). Fast help saves lives.
Testosterone replacement therapy is not recommended for men planning near-term fertility or for those with contraindications such as prostate cancer, markedly elevated PSA without urology evaluation, and untreated severe obstructive sleep apnea.
Men’s Health Is More Than a Number
This Men’s Health Month, make it personal: get curious, not complacent. Don’t accept feeling “off” as just part of getting older—track your symptoms, ask better questions, and partner with your clinician to look beyond a single lab value. When men take an active role in understanding their changing biology, they not only improve their energy and focus but also protect their most vital resource—their mental health. Start the conversation, schedule the check-up, and take the next step toward feeling fully yourself again.



